Types of Healthcare Providers
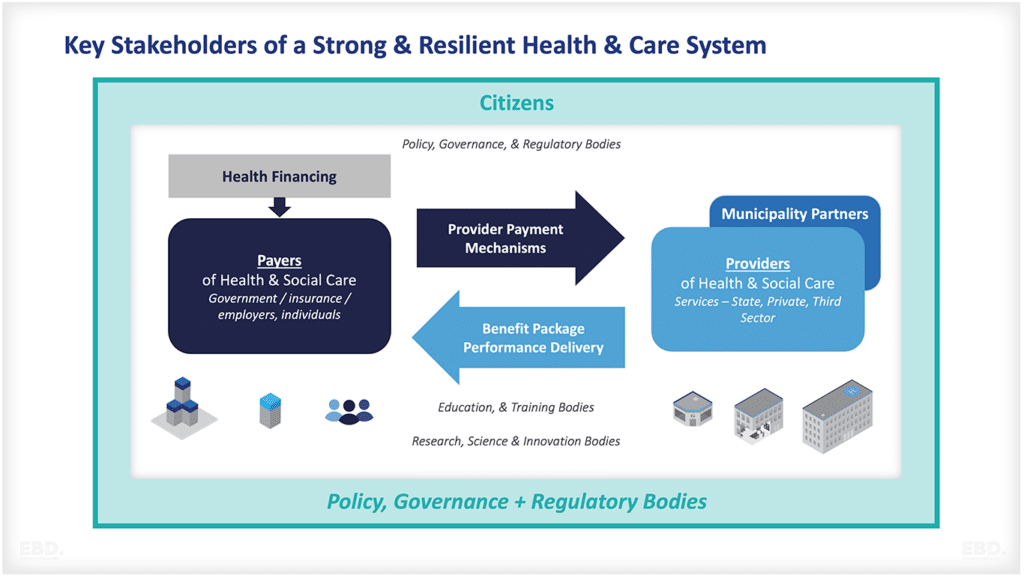
Individuals or those responsible for purchasing health services on behalf of a population (e.g. public or private health insurance companies or government purchasing agencies) will contract with a healthcare provider.
A healthcare provider can be any individual or organisation that delivers healthcare services.
The different types of healthcare providers can be categorised into two broad groups:
Individual Practitioners:
These are health professionals who are self-employed and work independently. Examples include GPs, consultants, dentists, optometrists and pharmacists.
Provider Organisations:
These are organisations that employ or contract with healthcare professionals and provide healthcare services. Examples include hospitals, GP practices, community pharmacies and dental surgeries.
This article looks at the different ownership structures of healthcare providers, examples of different types of healthcare providers, and key trends for consolidation and integration.
Who Owns Healthcare Providers?
There are a number of ownership models for the different types healthcare provider organisations. The three most common ownership models are:
Public Sector Providers:
These are providers that are owned and operated by the government.
Private Sector “for profit” Providers:
These are providers that are owned and operated by for-profit companies.
Private Sector “not-for-profit” Providers:
These are providers that are owned and operated privately but on a not-for-profit basis.
Most health systems have a mix of all three operating across all levels of care.
Publicly Owned Providers
The OECD defines publicly owned hospitals as “hospitals that are owned or controlled by a government unit or another public corporation (where control is defined as the ability to determine the general corporate policy)” OECD Health Statistics 2022.
The UK has the highest number of publicly owned hospitals in the OECD with the Netherlands having no hospitals in public ownership.
In the UK, hospitals are owned by either the National Health Service (NHS) or by local authorities. In the NHS in England, there are around 240 hospitals which are owned by NHS Foundation Trusts.
NHS Foundation Trusts are public sector organisations that operate in a similar way to private companies. They have more freedom than other NHS organisations to decide how they organise and deliver services. However, they still need to comply with NHS regulations.
Another example is the Netherlands where all hospitals are private but are not allowed to distribute funds to shareholders (owners) and so essentially operate as not-for-profit providers.
Publicly owned providers have a number of advantages and disadvantages. Some of the perceived advantages include:
- They usually operate free at the point of use which can increase access to care.
- They are accountable to the government which can improve transparency and quality.
- They can be more responsive to changes in government policy.
Some of the perceived disadvantages include:
- They can be less responsive to changes in consumer demand.
- They can be less efficient than private providers due to lower levels of competition.
- They can be less innovative than private providers.
Private Sector “for-profit” Providers
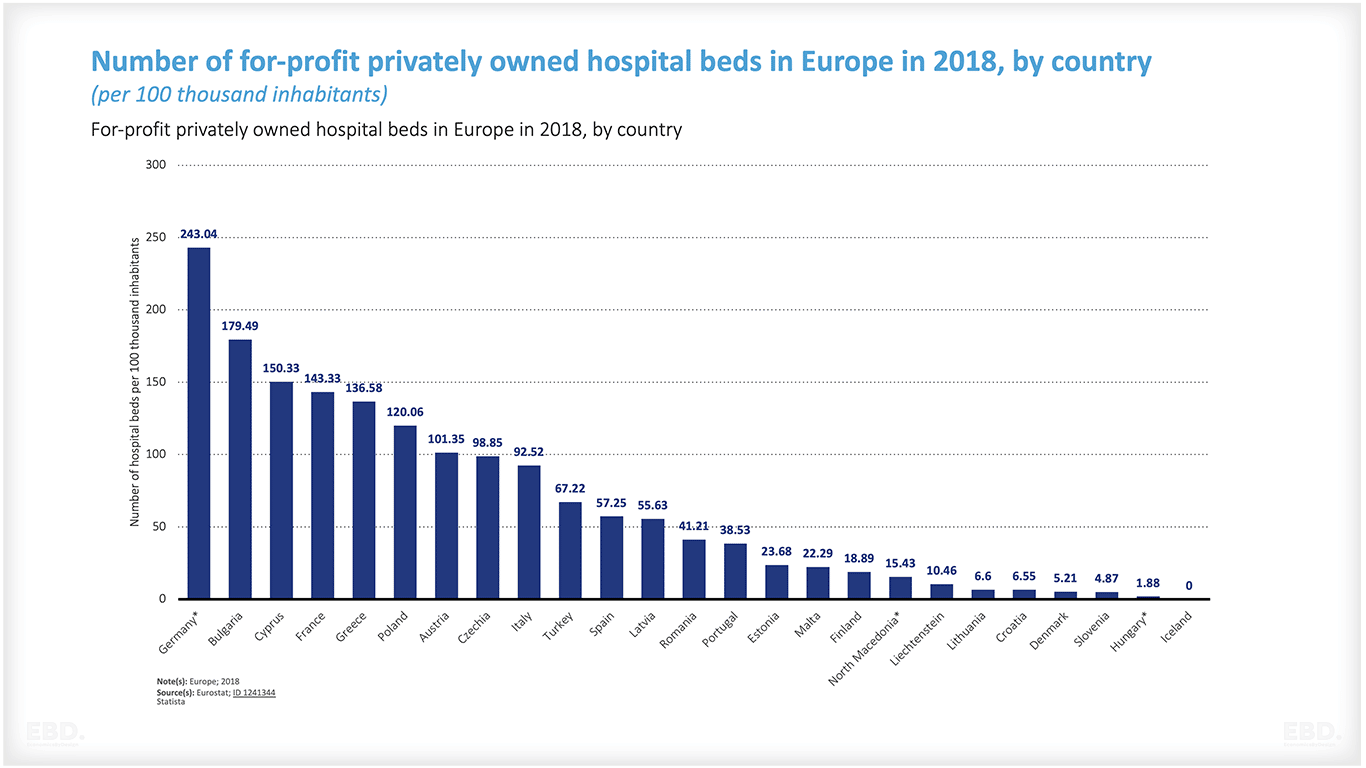
In the OECD, privately owned “for-profit” hospitals are defined as “Hospitals that are legal entities set up for the purpose of producing goods and services and are capable of generating a profit or other financial gain for their owners” (OECD Health Statistics 2022).
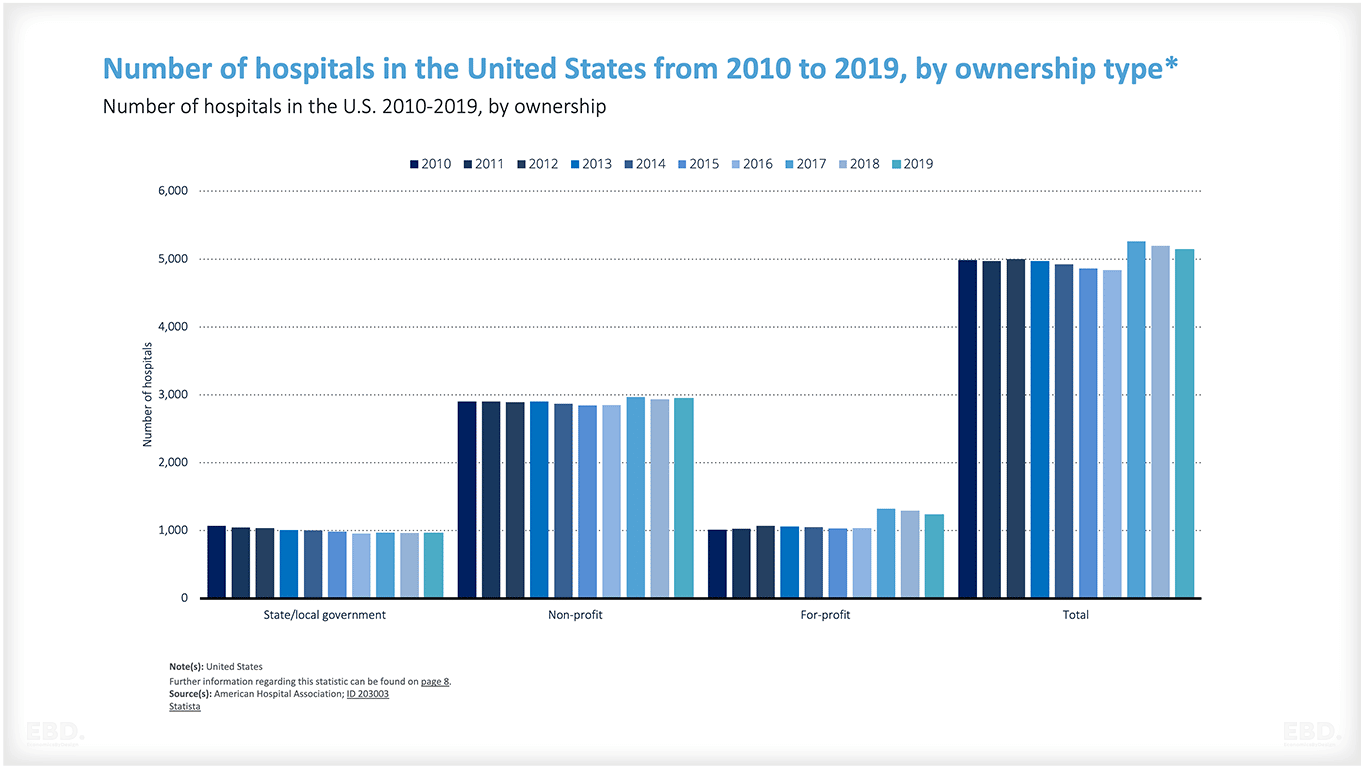
Examples of providers that are privately owned include Bupa and Nuffield Health in the UK. In the US, there are for-profit hospital chains such as HCA Healthcare. In India, the largest private healthcare services providers is Apollo Hospitals Enterprise Ltd. Countries with a high proportion of private hospitals include Chile, Colombia, Costa Rica, Mexico and Peru.
Primary care services are provided by the private sector in several countries. For example, in the UK, many GPs work in practices that are owned by private companies. In Australia, there are for-profit general practices known as medical centres.
Private Sector “not for profit” Providers
In the OECD, privately owned “not-for-profit” hospitals are defined as “legal or social entities created for the purpose of producing goods and services, whose status does not permit them to be a source of income, profit, or other financial gain for the unit(s) that establish, control or finance them”. (OECD Health Statistics 2022).
Privately owned not-for-profit hospitals are often established as charities or social enterprises. according to OECD statistics (2020), Korea has the highest reported rate of not-for-profit hospitals per million population. Some of the most famous hospitals in the USA are nonprofit and include the Mayo Clinic, Cleveland Clinic, and Johns Hopkins.
Just because a provider is described as “not for profit” doesn’t mean they are not profitable. A relatively recent study in Health Affairs showed that 7 out of the top 10 hospitals with the highest profit from patient services were “nonprofit”.
How Are Healthcare Providers Organised?
There are many different models for how healthcare providers can be organised.
Hospitals can be standalone organisations or they can be part of a larger system. For example, in the UK, most hospitals are owned by NHS Foundation Trusts which are separate legal entities from the NHS. In the US, hospitals can be part of a hospital system which is a collection of multiple hospitals that are owned by the same organisation.
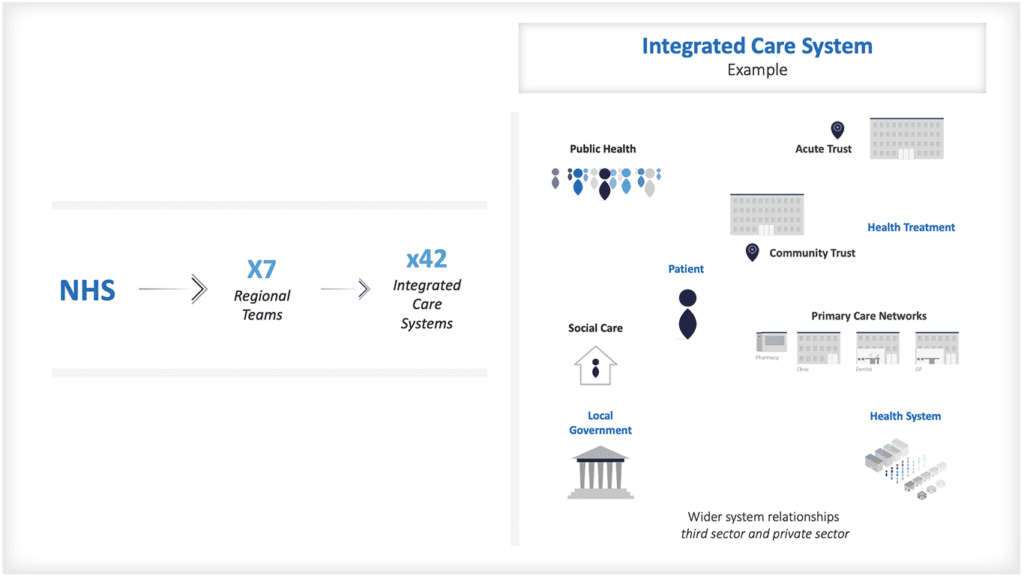
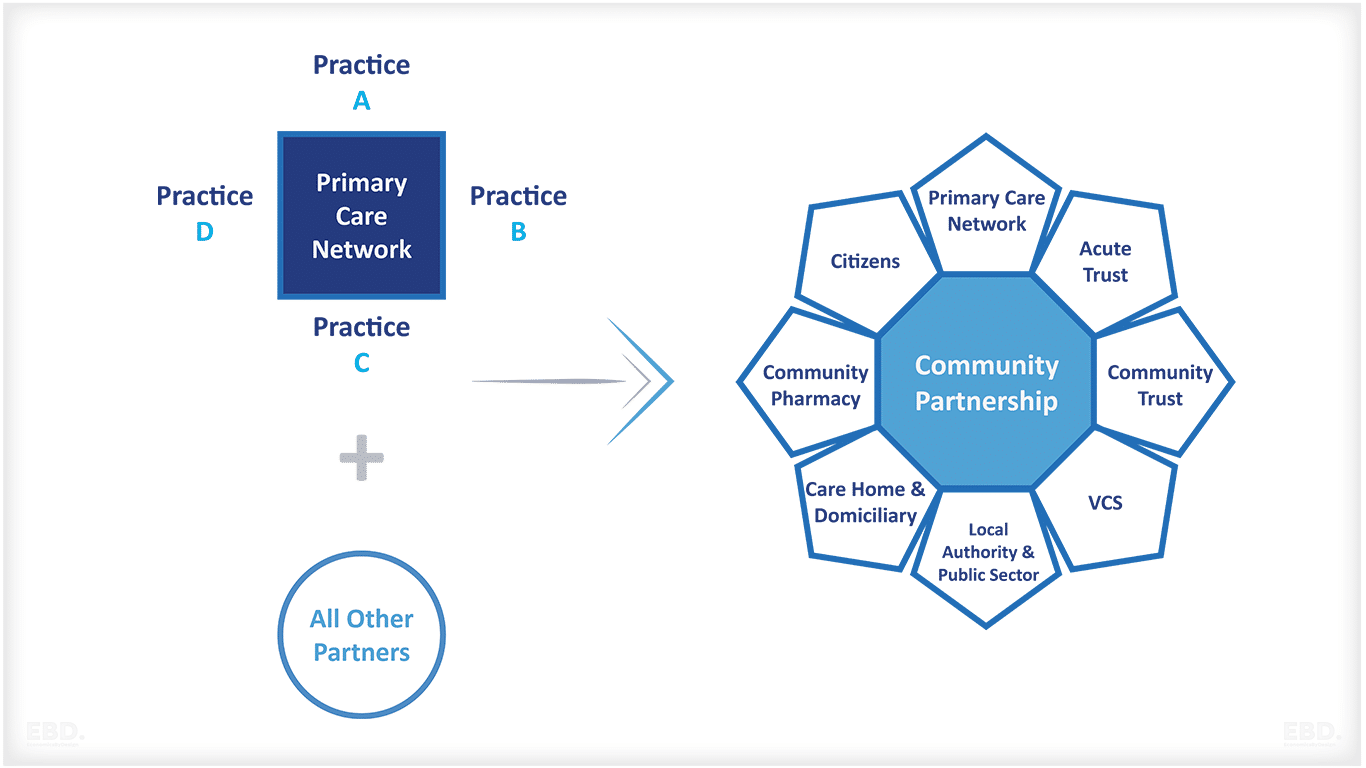
Primary care providers can also be standalone organisations or they can be part of a primary care network (PCN). PCNs are groups of general practices that work together to provide integrated care for their patients (NHS England, 2020).
In some countries, providers are organised into “provider groups”. These are defined as “autonomous, multi-professional organisations that are responsible and accountable for a population’s health needs” (OECD, 2016). Provider groups can be public, private or a mix of both.
What Are The Different Types Of Healthcare Providers?
There is huge diversity in healthcare organisations in terms of the services they cover (horizontal integration) and the degree of integration across levels of care (vertical integration). Here are some of the most common:
Accountable Care Organisations
An accountable care organisation (ACO) is a type of provider group that is common in the US. ACOs are “groups of doctors, hospitals, and other health care providers who come together voluntarily to give coordinated high-quality care to their Medicare patients” (Centers for Medicare and Medicaid Services, 2020).
Integrated Delivery Networks
An integrated delivery network (IDN) is another type of provider group that is common in the US. IDNs are “groups of hospitals, physicians, and other providers that have joined forces to provide coordinated, high-quality care” (American Hospital Association, 2020). IDNs can be public, private or a mix of both. One of the largest IDNs in the US is Partners HealthCare which is a private not-for-profit organisation.
Ambulatory Surgical Centres
An ambulatory surgical centre (ASC) is a type of provider that specialises in outpatient surgery. ASCs are commonly found in the US and they can be either for-profit or not-for-profit.
Physician-Hospital Organisation
A physician-hospital organisation (PHO) is a type of provider group that is common in the US. PHOs are “organisations consisting of one or more hospitals and a group of physicians who have joined forces to improve the quality and efficiency of care” (American Hospital Association, 2020).
PHOs can be public, private or a mix of both. One of the largest PHOs in the US is Mayo Clinic which is a private not-for-profit organisation.
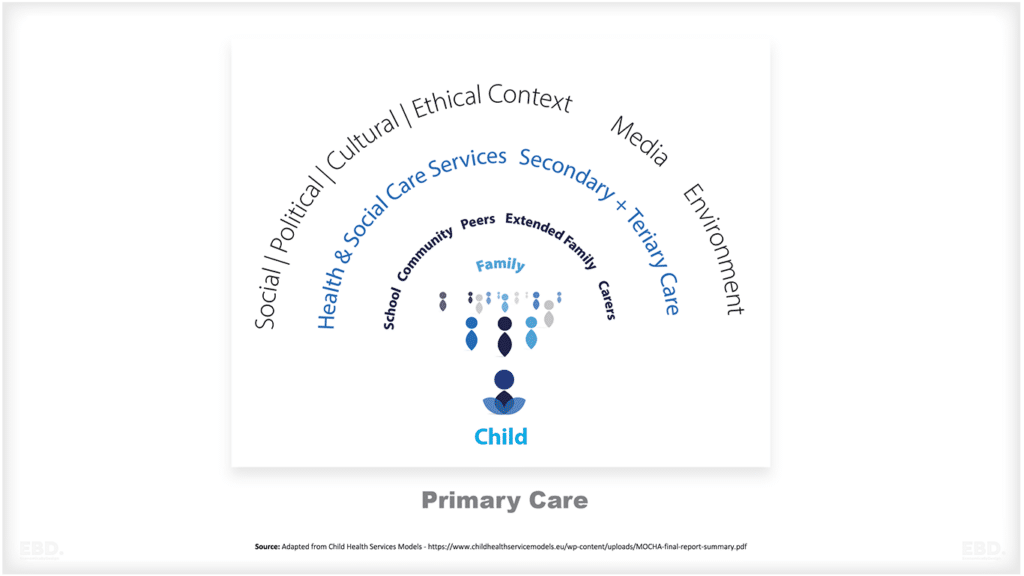
Patient-Centred Medical Homes
A patient-centred medical home (PCMH) is a type of primary care model that is common in the US since the Affordable Care Act (2010) and is increasingly common around the world. The key features of a PCMH are:
– A team-based approach to care
– A whole-person focus
– Comprehensive care
– Coordinated care
– Accessible care
Primary Care Networks
A primary care network (PCN) is a type of provider group that is common in the UK. PCNs are “groups of general practices that work together to provide integrated care for their patients” (NHS England, 2020).
The UK has the highest number of publicly owned hospitals in the OECD with the Netherlands having no hospitals in public ownership.
In the UK, hospitals are owned by either the National Health Service (NHS) or by local authorities. In the NHS in England, there are around 240 hospitals which are owned by NHS Foundation Trusts.
NHS Foundation Trusts are public sector organisations that operate in a similar way to private companies. They have more freedom than other NHS organisations to decide how they organise and deliver services. However, they still need to comply with NHS regulations.
Another example is the Netherlands where all hospitals are private but are not allowed to distribute funds to shareholders (owners) and so essentially operate as not-for-profit providers.
Publicly owned providers have a number of advantages and disadvantages. Some of the perceived advantages include:
- They usually operate free at the point of use which can increase access to care.
- They are accountable to the government which can improve transparency and quality.
- They can be more responsive to changes in government policy.
Some of the perceived disadvantages include:
- They can be less responsive to changes in consumer demand.
- They can be less efficient than private providers due to lower levels of competition.
- They can be less innovative than private providers.
Private Sector “for-profit” Providers
In the OECD, privately owned “for-profit” hospitals are defined as “Hospitals that are legal entities set up for the purpose of producing goods and services and are capable of generating a profit or other financial gain for their owners” (OECD Health Statistics 2022).
Examples of providers that are privately owned include Bupa and Nuffield Health in the UK. In the US, there are for-profit hospital chains such as HCA Healthcare. In India, the largest private healthcare services providers is Apollo Hospitals Enterprise Ltd. Countries with a high proportion of private hospitals include Chile, Colombia, Costa Rica, Mexico and Peru.
Primary care services are provided by the private sector in several countries. For example, in the UK, many GPs work in practices that are owned by private companies. In Australia, there are for-profit general practices known as medical centres.
Private Sector “not for profit” Providers
In the OECD, privately owned “not-for-profit” hospitals are defined as “legal or social entities created for the purpose of producing goods and services, whose status does not permit them to be a source of income, profit, or other financial gain for the unit(s) that establish, control or finance them”. (OECD Health Statistics 2022).
Privately owned not-for-profit hospitals are often established as charities or social enterprises. according to OECD statistics (2020), Korea has the highest reported rate of not-for-profit hospitals per million population. Some of the most famous hospitals in the USA are nonprofit and include the Mayo Clinic, Cleveland Clinic, and Johns Hopkins.
Just because a provider is described as “not for profit” doesn’t mean they are not profitable. A relatively recent study in Health Affairs showed that 7 out of the top 10 hospitals with the highest profit from patient services were “nonprofit”.
How Are Healthcare Providers Organised?
There are many different models for how healthcare providers can be organised.
Hospitals can be standalone organisations or they can be part of a larger system. For example, in the UK, most hospitals are owned by NHS Foundation Trusts which are separate legal entities from the NHS. In the US, hospitals can be part of a hospital system which is a collection of multiple hospitals that are owned by the same organisation.
Primary care providers can also be standalone organisations or they can be part of a primary care network (PCN). PCNs are groups of general practices that work together to provide integrated care for their patients (NHS England, 2020).
In some countries, providers are organised into “provider groups”. These are defined as “autonomous, multi-professional organisations that are responsible and accountable for a population’s health needs” (OECD, 2016). Provider groups can be public, private or a mix of both.
What Are The Different Types Of Healthcare Providers?
There is huge diversity in healthcare organisations in terms of the services they cover (horizontal integration) and the degree of integration across levels of care (vertical integration). Here are some of the most common:
Accountable Care Organisations
An accountable care organisation (ACO) is a type of provider group that is common in the US. ACOs are “groups of doctors, hospitals, and other health care providers who come together voluntarily to give coordinated high-quality care to their Medicare patients” (Centers for Medicare and Medicaid Services, 2020).
Integrated Delivery Networks
An integrated delivery network (IDN) is another type of provider group that is common in the US. IDNs are “groups of hospitals, physicians, and other providers that have joined forces to provide coordinated, high-quality care” (American Hospital Association, 2020). IDNs can be public, private or a mix of both. One of the largest IDNs in the US is Partners HealthCare which is a private not-for-profit organisation.
Ambulatory Surgical Centres
An ambulatory surgical centre (ASC) is a type of provider that specialises in outpatient surgery. ASCs are commonly found in the US and they can be either for-profit or not-for-profit.
Physician-Hospital Organisation
A physician-hospital organisation (PHO) is a type of provider group that is common in the US. PHOs are “organisations consisting of one or more hospitals and a group of physicians who have joined forces to improve the quality and efficiency of care” (American Hospital Association, 2020).
PHOs can be public, private or a mix of both. One of the largest PHOs in the US is Mayo Clinic which is a private not-for-profit organisation.
Patient-Centred Medical Homes
A patient-centred medical home (PCMH) is a type of primary care model that is common in the US since the Affordable Care Act (2010) and is increasingly common around the world. The key features of a PCMH are:
– A team-based approach to care
– A whole-person focus
– Comprehensive care
– Coordinated care
– Accessible care
Primary Care Networks
A primary care network (PCN) is a type of provider group that is common in the UK. PCNs are “groups of general practices that work together to provide integrated care for their patients” (NHS England, 2020).
NHS Foundation Trusts
NHS Foundation Trust (NFT) is a type of provider in England that provides NHS hospital and or community health services. NFTs are “autonomous, publicly accountable organisations” that “operate within the NHS and are free from day-to-day Government control” (NHS Foundation Trusts, 2020). NHS Foundation Trusts often operate across multiple hospital and community sites.
Academic Health Science Centres
An academic health science centre (AHSC) is a type of provider that is common in the US, UK and Canada. AHSCs are “universities and teaching hospitals that have joined forces to improve the quality of patient care, advance medical education and training, and conduct groundbreaking research” (Association of American Medical Colleges, 2020).
Military Hospitals
These are hospitals that are run by the military and they provide care to members of the armed forces and their families. Military hospitals are found in many countries around the world.
Trends Towards Provider Consolidation
There has been a trend towards consolidation in the healthcare sector in recent years. This means that there have been an increasing number of provider groups and an increase in the size of these groups. The reasons for this consolidation are:
– To improve quality of care
– To reduce costs
– To increase efficiency
– To improve access to care
The trend towards consolidation is likely to continue in the future as provider groups look for ways to increase their scale and scope.
Provider Organisation & Integrated Care
There is an increasing trend towards the use of Strategic Purchasing to ensure providers work together to deliver integrated care. Examples of how providers have responded include the establishment of accountable care organisations, integrated delivery networks and the increasing tendency for primary care practitioners to be linked or affiliated to hospital systems.
There is also a trend towards integration between healthcare purchasing and healthcare provision. Here are some examples:
Managed Care Organisation
A managed care organisation (MCO) is a type of provider group that provides healthcare services to a group of enrollees. MCOs are common in the US and they can be either for-profit or not-for-profit. They are sometimes referred to as integrators as they may commonly work at the interface between insurance funds and service providers for the delivery of care.
Health Maintenance Organisations
A health maintenance organisation (HMO) is a specific type of managed care organisation. They work on the principle of providing care to a population for a fixed price.
The first HMO was established in USA, in 1929, the Ross-Loos Medical Group. International examples include Isreal which has regionally based HMOs and all residents have to be registered with at least one. Other examples include the Philippines and Nigeria.
HMOs have different operating models; they can employ staff and deliver care, contract with self-employed or groups of health professionals to deliver care or contract with a network of providers to secure care.
How Can Health Care Providers Improve Economic Value?
The delivery of health services is the core function of a healthcare system. Healthcare providers, therefore, have a huge role to play in ensuring that the resources are used effectively and efficiently and deliver value:
- by improving quality and improving healthcare outcomes
- by delivering services safely and ensuring patients receive the right treatment at the right time and are not exposed to health risks such as infections
- by controlling costs
- by increasing productivity and efficiency in the use of resources
- by improving access to healthcare
Strategic Purchasing and Provider Payment Models can support and encourage providers to increase value, such that the system as a whole can deliver value-based care.
Useful References
Association of American Medical Colleges. (2020). Academic Health Science Centers.
NHS England. (2019). Integrated care partnerships: Overview and guidance for STPs and ICSs.
Ross, J. M., & Loos, W. H. (1929). A new type of medical practice: the group practice without a hospital. New England Journal of Medicine, 201(17), 788-793.
U.S. Department of Health and Human Services. (n.d.). What is an HMO?
Wolters Kluwer. (2018). Consolidation in the healthcare industry: Drivers, benefits and challenges.