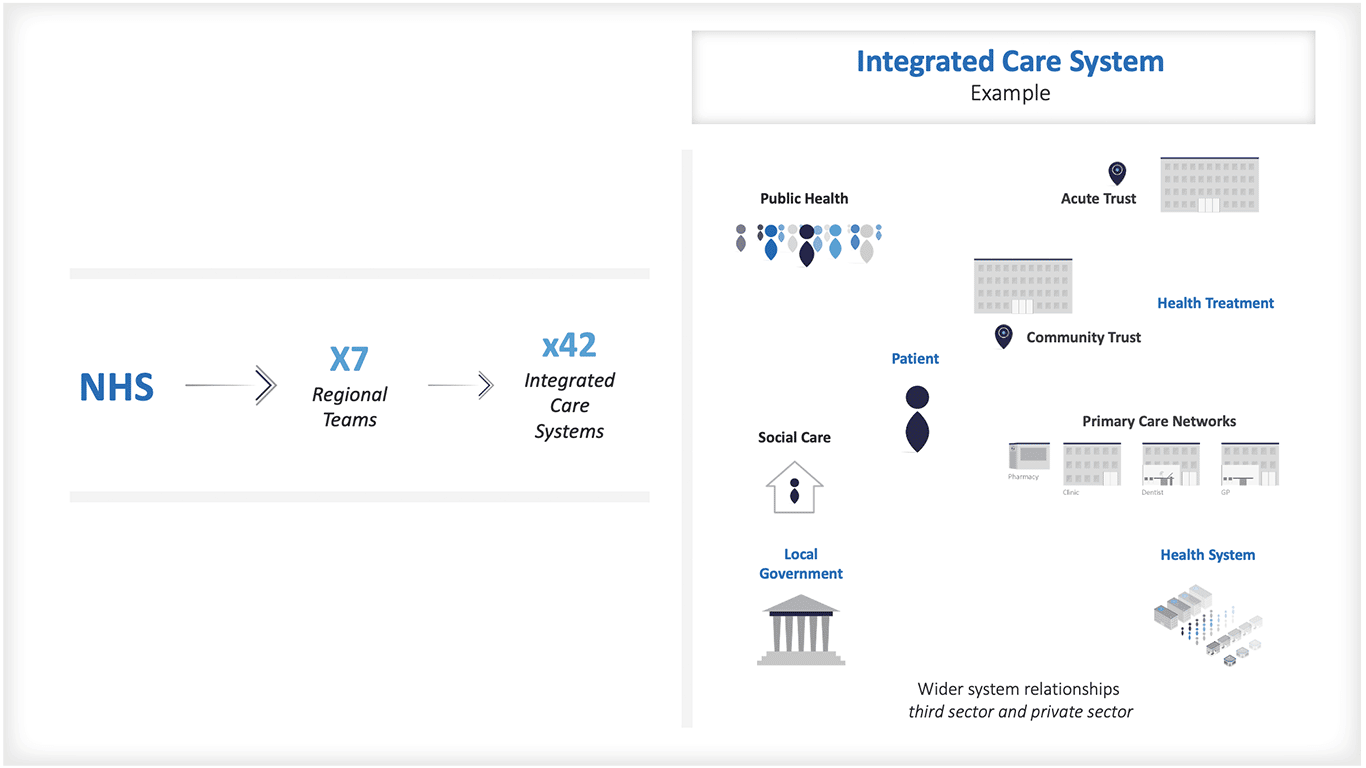
Integrated Care Systems
The new integrated care systems being established across England have ambitious goals to improve health and wellbeing outcomes and to oversee the delivery of properly joined-up health and care services.
Integrated Care Boards will need to think carefully about how funding will flow to NHS organisations and their partners at the front line to pay for the right resources, in the right place, at the right time.
How will integrated care systems work?
The NHS Long-term Plan and the Health and Care Act (2022) position integrated care systems at the centre of health system reform.
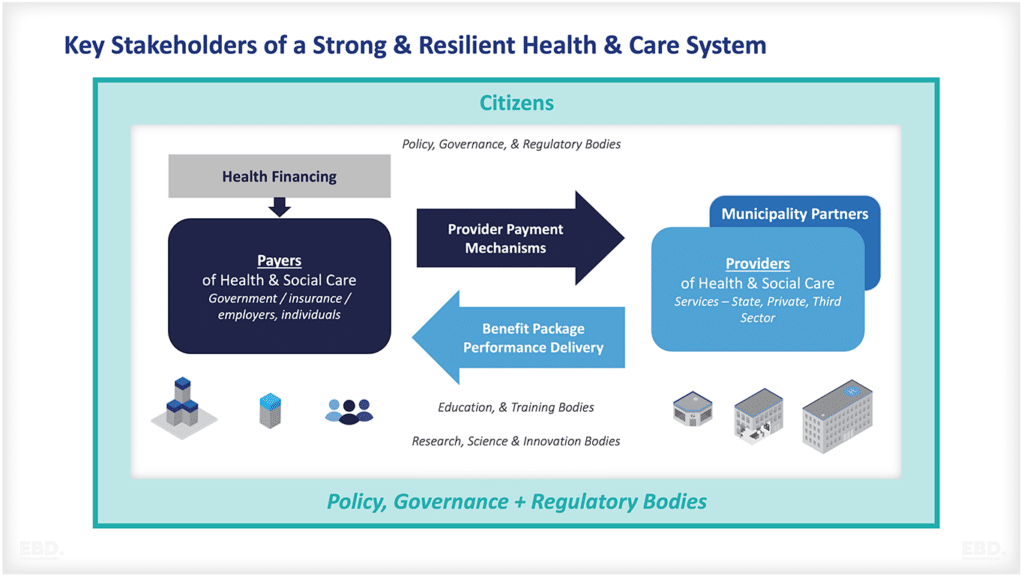
They are partnerships which bring together providers and commissioners of health and care services across geographical areas to collectively improve population health and health and care coordination.
How many integrated care systems are there in the UK?
There are 42 integrated care systems covering the NHS in England.
What is the difference between strategic transformation partnerships and integrated care systems?
Strategic Transformation Partnerships (STP) were established as part of the NHS Long-Term Plan. NHS England and NHS Improvement redesigned the integrated care systems in the 2018/19 planning guidance. All STPs have been incorporated into integrated care systems.
Why were integrated care systems created?
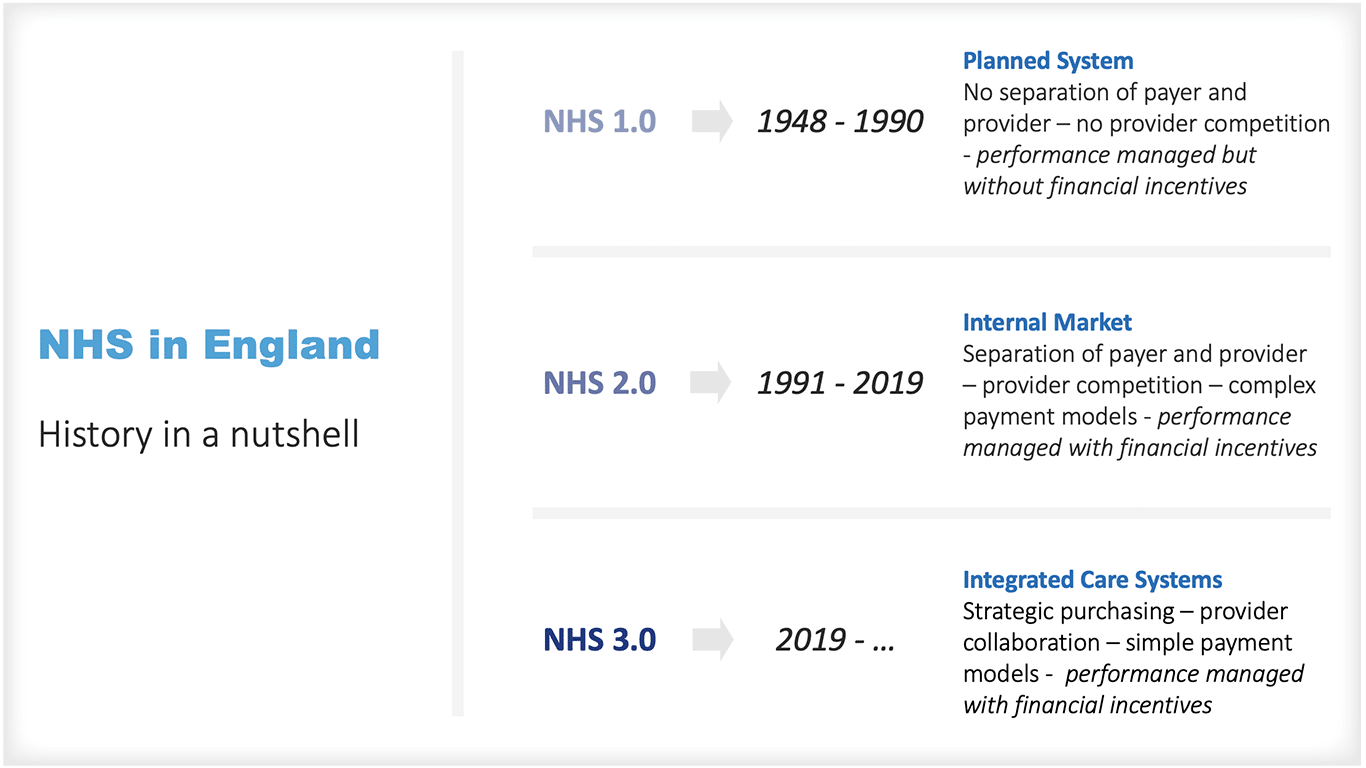
Following its creation in 1948, the NHS was largely a tax-funded, government-managed, hospital and community health system, supported by independent general practitioners.
The public sector transformation which took place in the 1980s saw the privatisation of many former public services. The then government stopped short of privatising the health service but did create the ‘internal market’ for health. This has characterised the NHS operating model in England for the last three decades.
Working for Patients, launched in 1991 saw the creation of NHS organisations responsible for buying services on behalf of patients and citizens (ultimately becoming known as Clinical Commissioning Groups) and NHS organisations responsible for providing health and care services.
This new health care system was designed to improve efficiency, decentralise decision making, increase the patient responsiveness of NHS providers, and improve accountability, management information and ‘customer service’.
We have seen many reorganisations of the internal market since 1991 as the design of the internal market has been adjusted to respond to the new challenges and complexities it created.
Ultimately, the NHS Long-Term Plan took the best of the internal market but adapted it to address what had become long-standing system challenges of health inequalities and poor coordination.
These problems had been exacerbated, at least in part, by the perverse incentives created by payment models which rewarded NHS providers for high volume hospital-based care.
What are integrated health system goals?
They exist to achieve four aims:
1. Improve outcomes in population health and healthcare
2. Tackle inequalities in outcomes, experience and access
3. Enhance productivity and value for money
4. Help the NHS support broader social and economic development
What were NHS funding flows and payment models?
The internal market saw the introduction of tariff-based payments to NHS providers for NHS services.
These payment models were initially introduced to deal with the prevailing problems of large and long waiting lists for planned surgery. However, it soon became clear that ‘payment by results’ might lead to an over-reliance on hospital care. They did little to reward quality and health outcomes, and nothing to improve population health. More fundamentally they failed to help the health and care sector to tackle health inequalities.
As the internal market developed, so too did a wider and deeper and increasingly complex system of payment models and corrections to the perverse incentives they created.
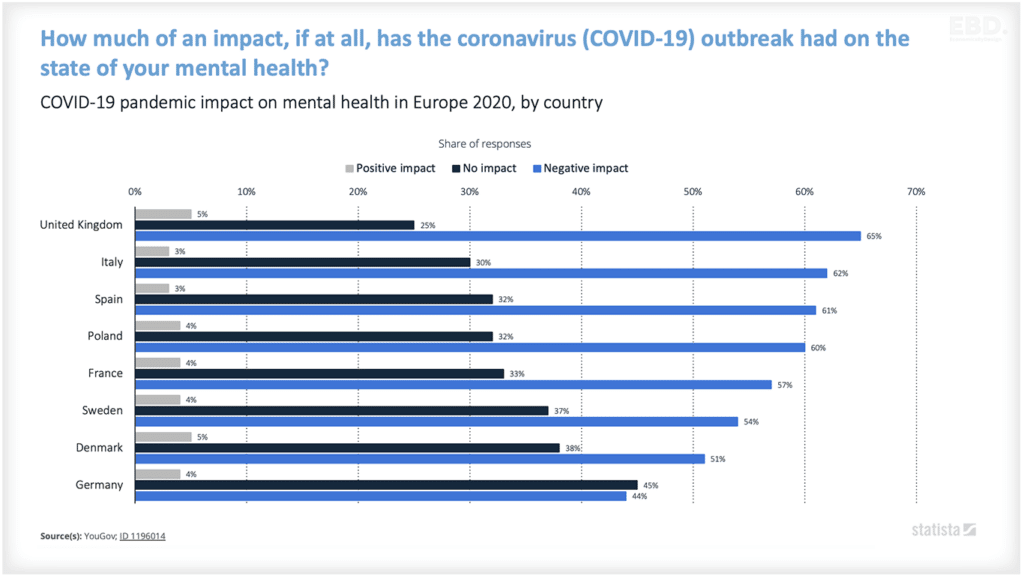
The last two years, turbocharged by COVID-19 pressures, marked an end to the dominance of tariff-based payment mechanisms that characterised the internal market. Since March 2020 the former complexity has all gone, as has the associated immense administrative burden.
The pandemic saw an accelerated move to financial performance being monitored at the health and care system level, with clinical commissioning groups having their budgets aggregated for the health and care system. For NHS providers, there was an immediate move to block contracts based on rolling costs.
Integrated Care Systems & Payment Models
Budgetary responsibilities
The integrated care board will control almost all local NHS budgets, except for some of the specialized NHS funding held by NHS England to pay for specialist services.
Wide remit
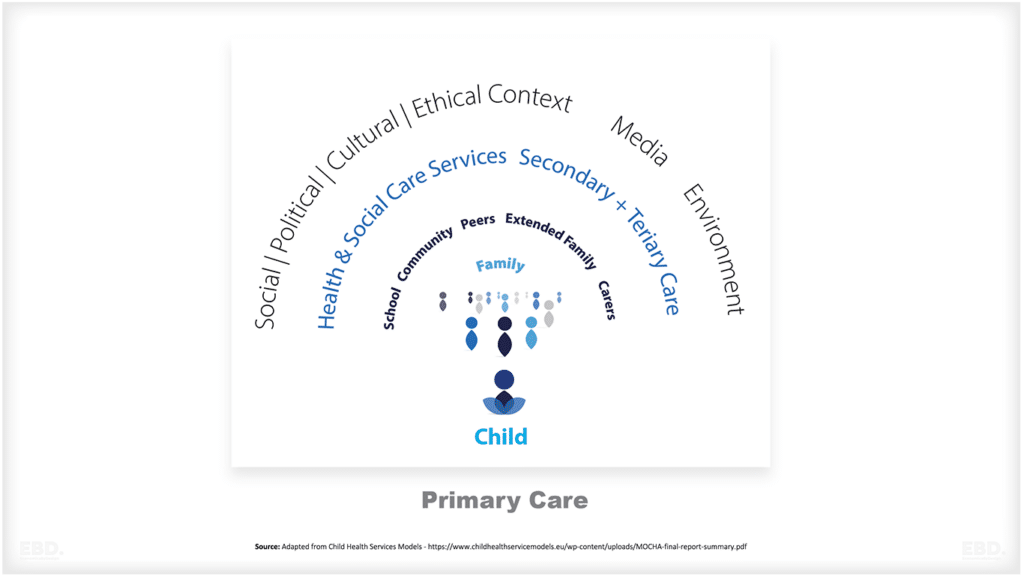
Integrated care systems should not just be interested in paying for hospital and community health services; their goals are also linked to the success and quality of primary healthcare, public health and related expenditure, and social care funding.
Opportunities to align spending priorities across the NHS and local authorities will be enhanced, particularly for defined geographical areas (known as ‘place’) and geographically-based communities within them (known as ‘neighbourhoods’).
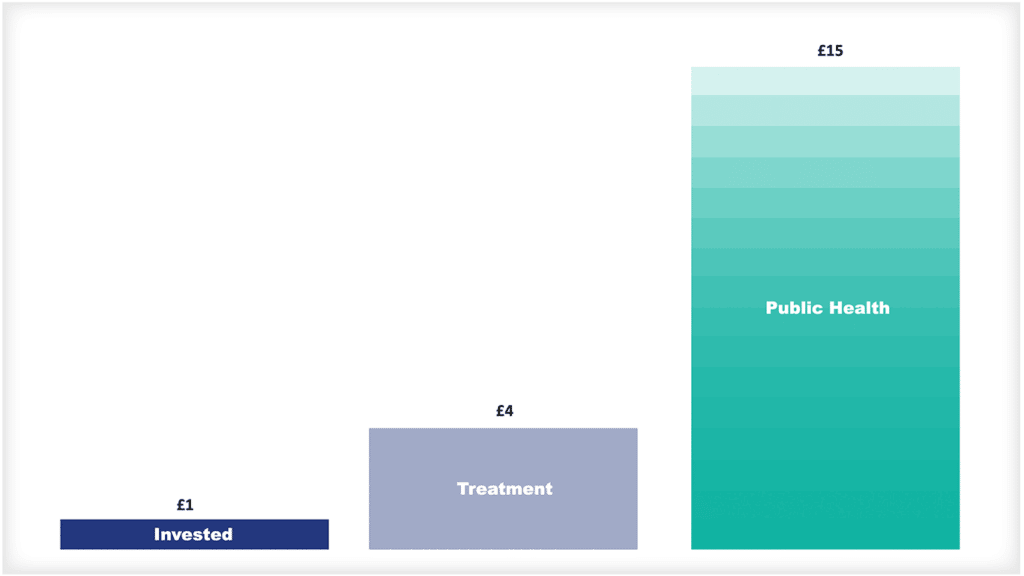
Strategic funding imbalance
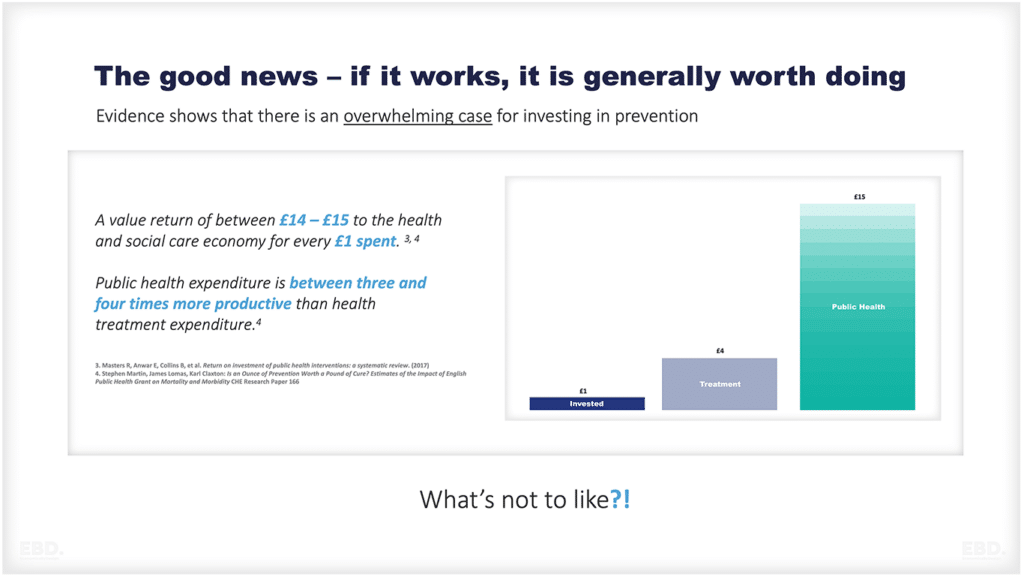
There will be limits to this. There has been inadequate national investment in measures improving population health, that tackle health inequalities, and in fragmented patient care pathways.
This has resulted in a strategic misalignment between funding flows for hospital and community health services and funding for those partner organisations that play a pivotal role in achieving population health goals and integrated health and social care.
The health and care act (2022) will not resolve this issue.
How should an Integrated Care System use payment models to achieve their goals?
An integrated care system will need to ensure that money is available at the front line to pay for the right resources in the right place at the right time in support of their goals.
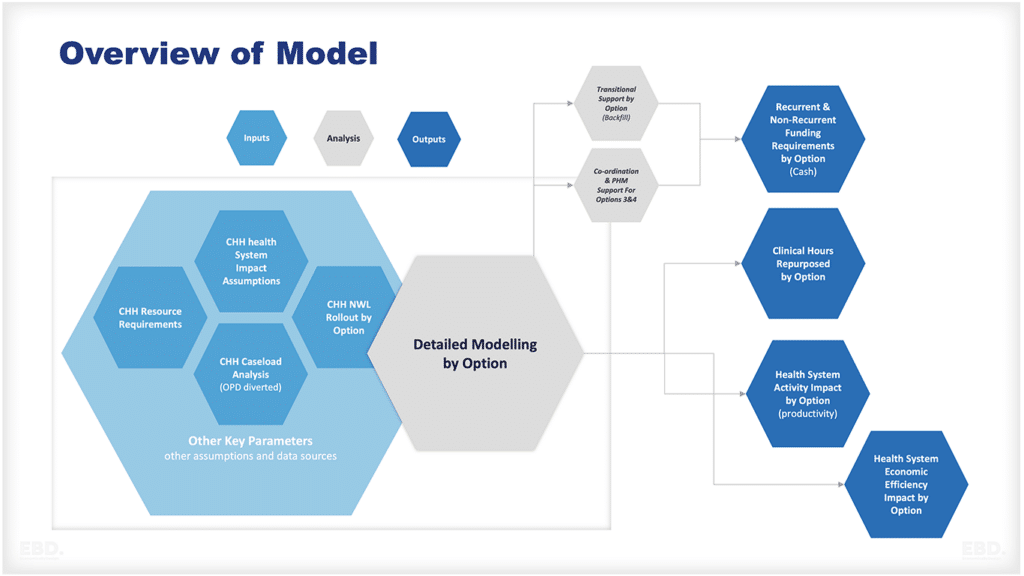
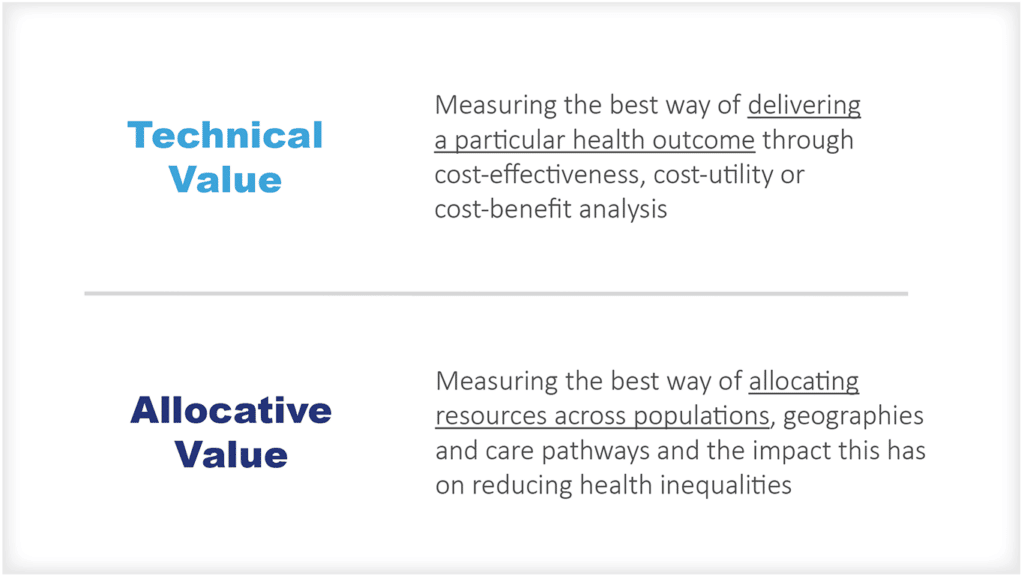
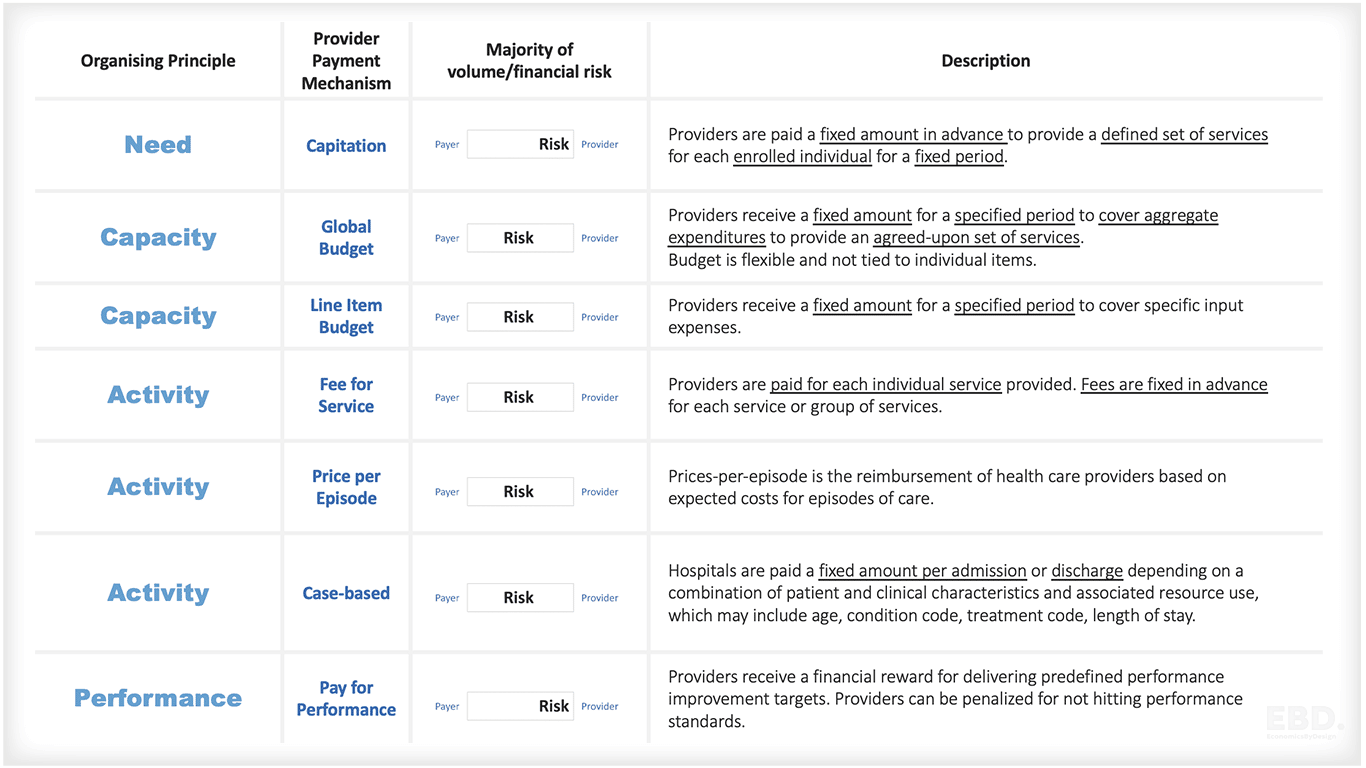
Work by Economics By Design on a project based in Sudan for the World Health Organisation, examined five core design principles which influence the choice of payment models: needs, capacity, activity, performance, and outcomes.
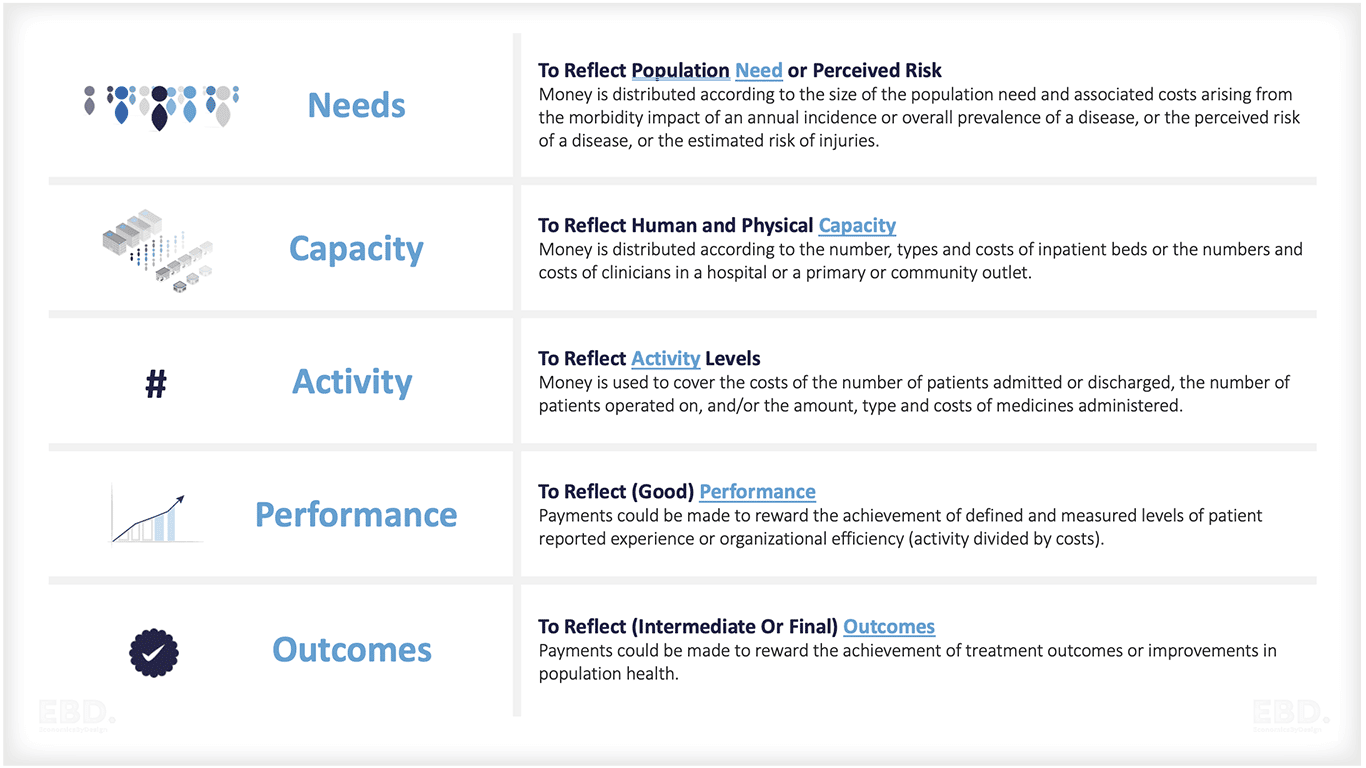
NEEDS
The Opportunity
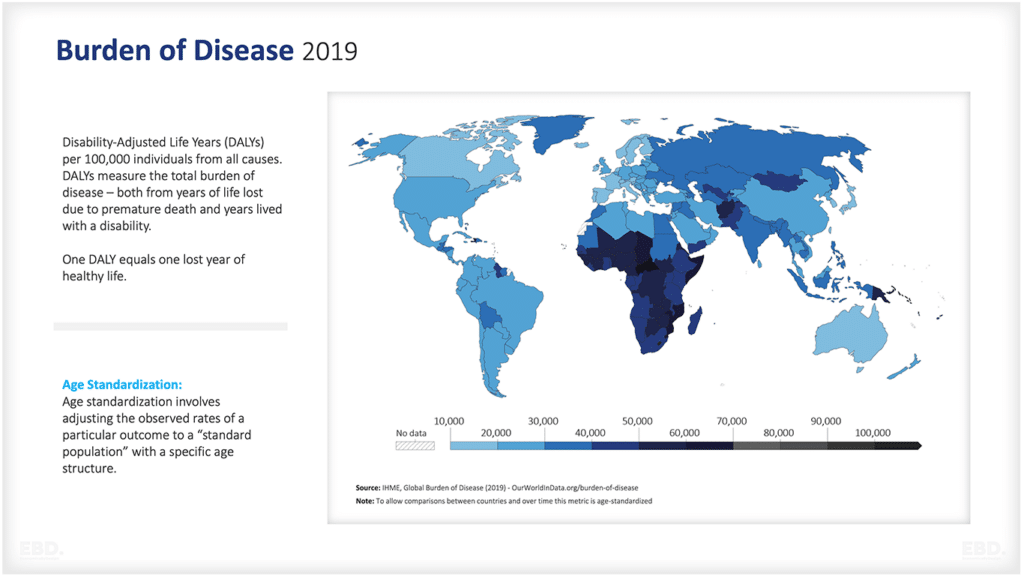
Needs-based models are used where payment is distributed according to the size of the population need and associated costs arising from the impact or illness impact of an annual incidence or overall prevalence of a disease, or the perceived risk of a disease, or risk of injuries.
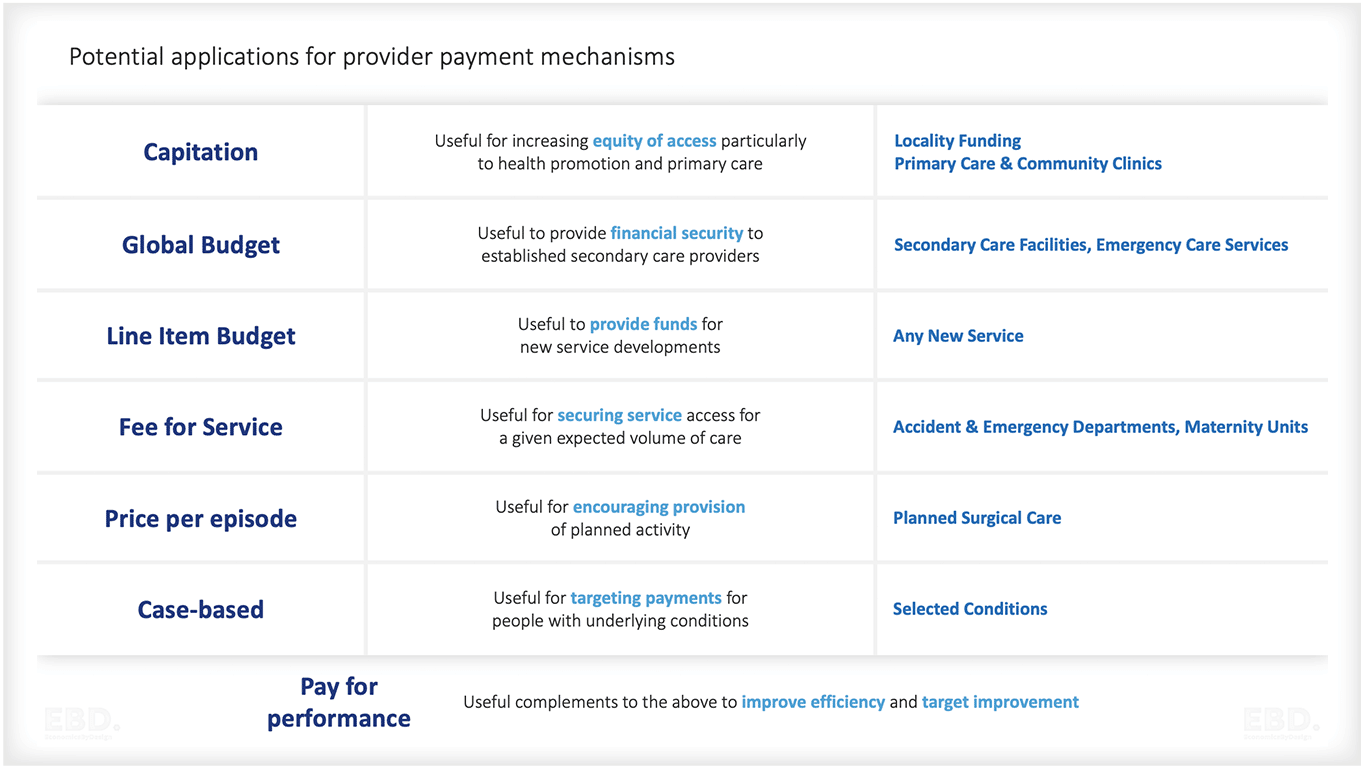
Capitation is an example of a payment system designed to address need and/or relative need.
The Challenge
If you’re paying solely on the basis of need it can be quite difficult to mobilise supply, it involves effectively giving out a budget based on what you think is needed but it doesn’t specifically incentivise improved supply or delivery or quality.
CAPACITY
The Opportunity
Here, money is distributed according to the number, types and costs of inpatient beds or the numbers and costs of clinicians in a hospital or a primary or community outlet.
Examples here include Global Budgets, Line Item Budget (often enshrined in “Block” contracts).
The Challenge
For payment mechanisms that are designed solely around capacity, it can become very difficult to increase utilisation and to mobilise improvement.
ACTIVITY
The Opportunity
Payments can be used to reimburse providers according to the number of patients admitted or discharged, operated on, and/or the amount, type and costs of medicines administered.
This can include Fee for Service payments, Price per Episode, or Case-Based payments such as DRG or HRG-based tariffs.
The Challenge
Mechanisms focused solely on activity can result in over-treatment and, if not capped, can lead payers to exceed their budgets very quickly.
PERFORMANCE
The Opportunity
This involves payments designed to reward the achievement of defined and measured levels of patient-reported experience or organizational efficiency (activity divided by costs).
Examples here include Best Practice Tariffs.
The Challenge
Payments that are exclusively geared towards rewarding performance can be become quite complex and interact badly. The system can end up being characterised by perverse incentives increasing costs and reducing quality.
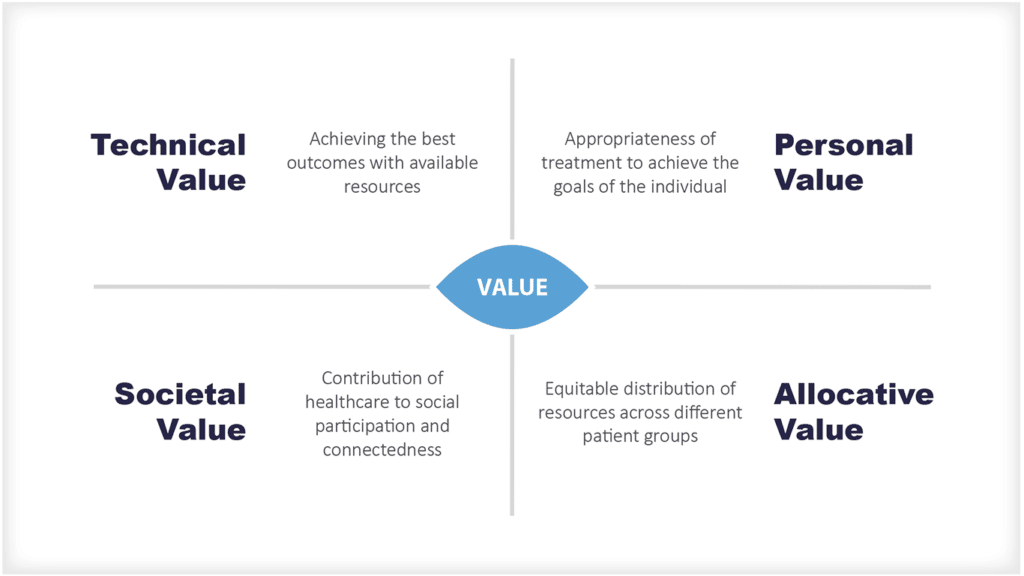
OUTCOMES
The Opportunity
Payments can be geared to reward the achievement of treatment outcomes, patient experience, or even improving population health. Outcome-Based Payment models fall into this category.
There remains much discussion about the feasibility of a longer-term move towards a population health approach advocated as part of value-based healthcare and supported by value-based payment models, but the search for the payment model nirvana continues.
The Challenge
Payments based solely on outcomes are really not sustainable for small organisations who actually need to pay the bills whilst delivering.
More fundamentally, it is also not always easy to attribute cause and effect, and there are many contributory factors that impact outcomes which have nothing to do with provider performance.
Blended Payment Models
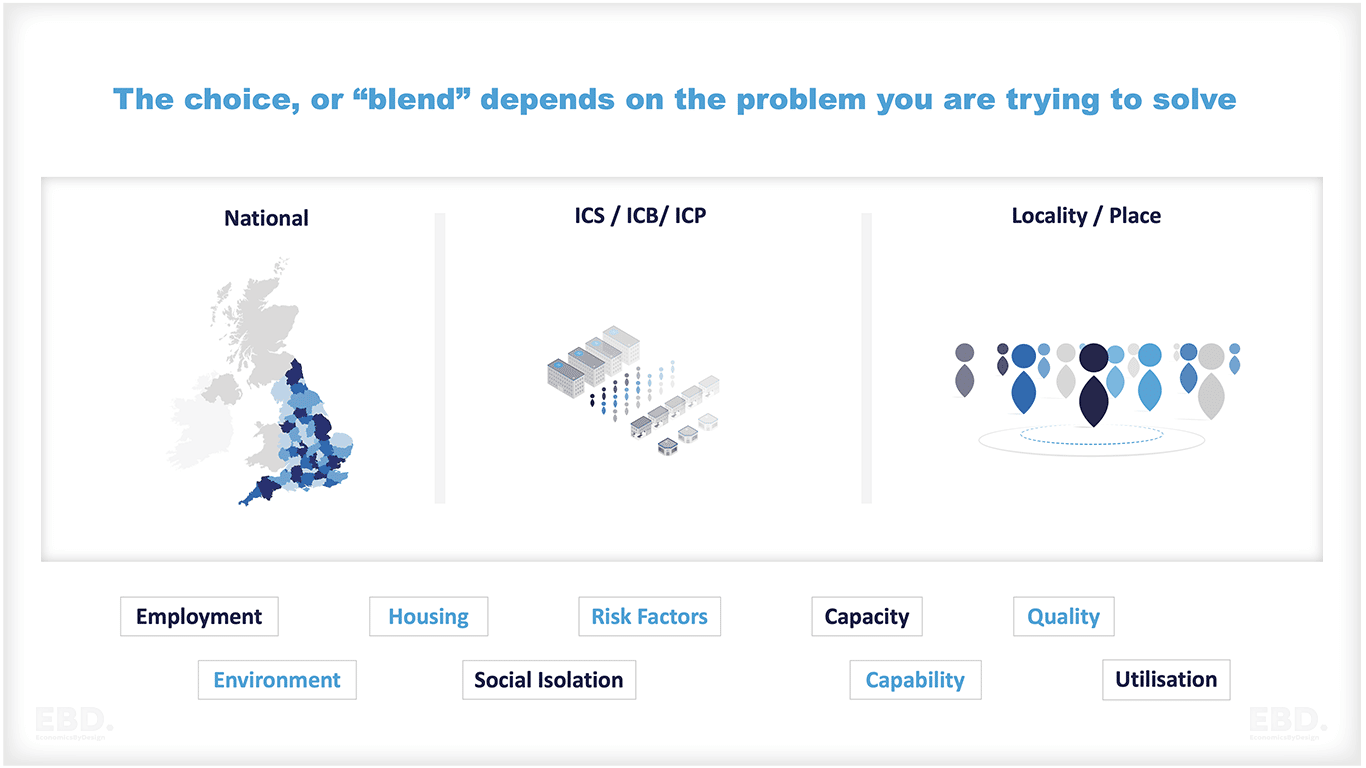
There is clearly no magic bullet and in practice, many countries have adopted combinations of models to suit local circumstances and to address specific problems about increasing capacity, utilisation and improving quality and outcomes.
A new aligned payment and incentive approach has already been introduced in the NHS in England. It is a precursor to the more flexible blended payment models which are expected to develop as the new health and care system matures.
The payment models included in the health and care act (2022) will set new parameters within which integrated care boards can operate. These will reduce bureaucracy and will promote the treatment of patients in primary and community care settings.
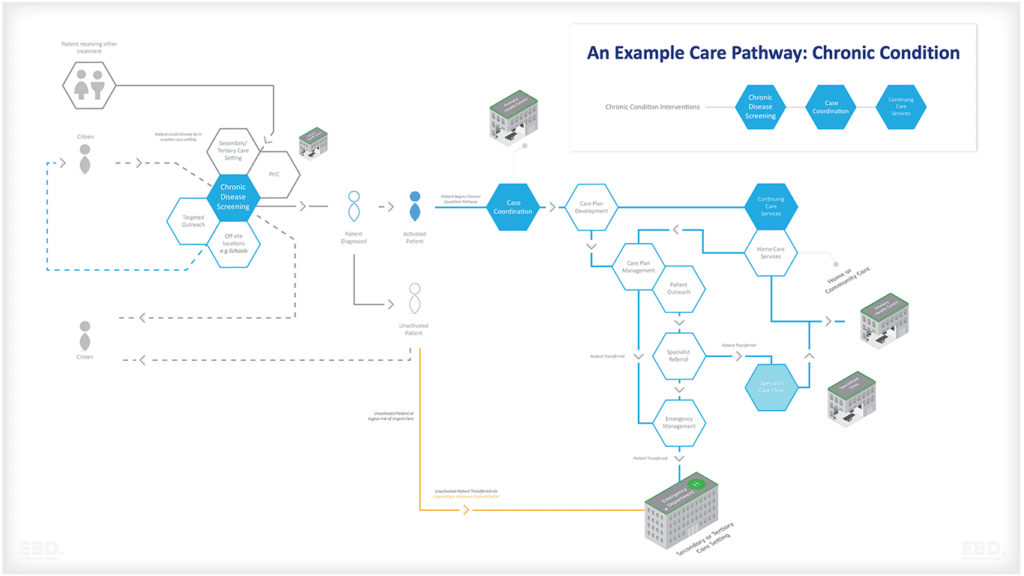
The new models will enable payment for whole pathways of care. Importantly, they will enable payment for programmes of prevention and population health as part of pathways for care.
Moving forwards
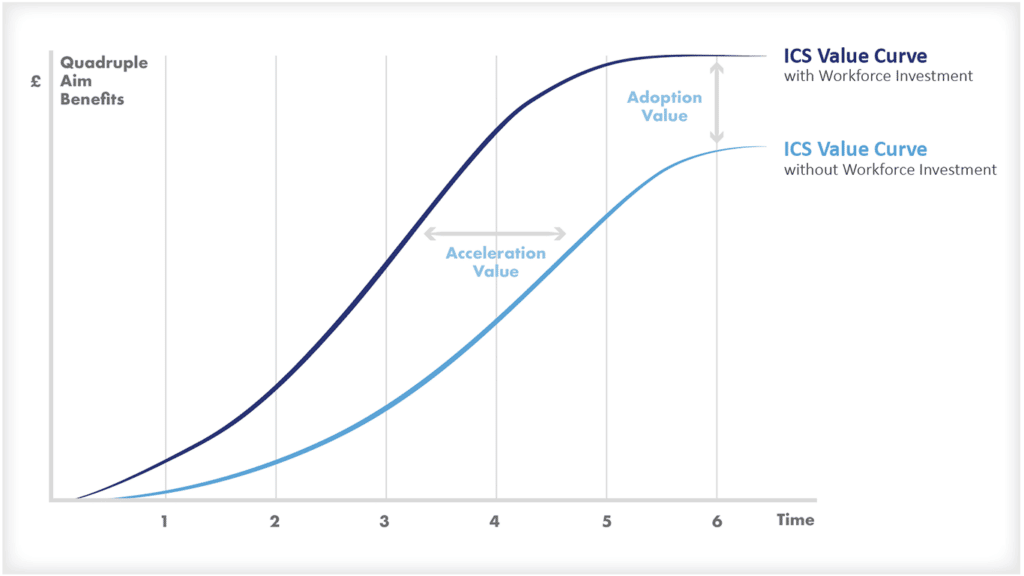
Integrated care systems have already been given a lot more flexibility to determine how funding flows, than existed under the internal market. As they mature, and use these flexibilities to solve the local problem faced, they will need to pay attention to payment models as positive levers for achieving their goals.
Integrated care boards will have a genuine opportunity to use the design principles of need, capacity, activity, performance and outcomes, to work within national guidelines to design well-targeted methods of allocating funds and paying for services to providers and indeed across the system.