Essential Health Benefits
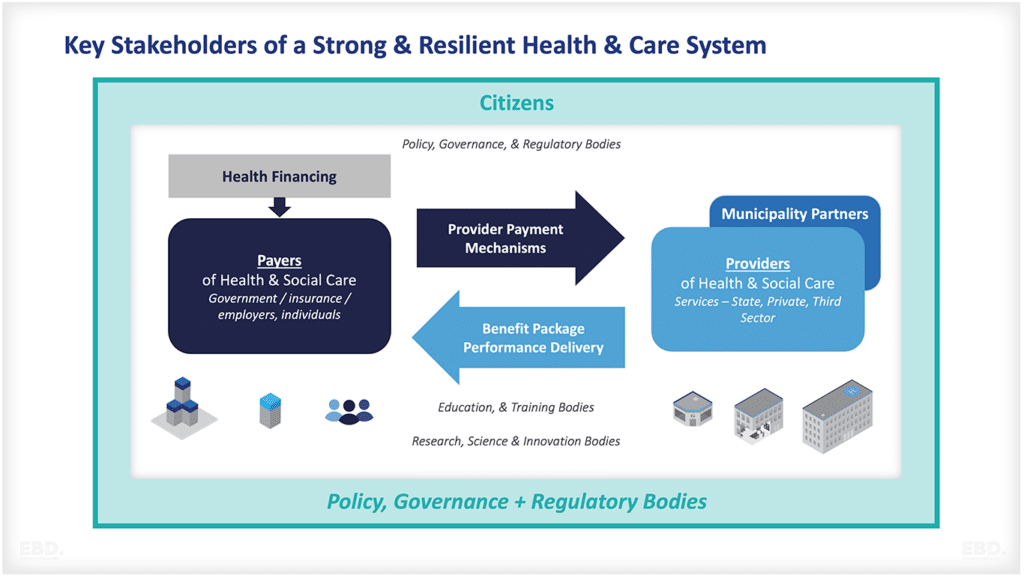
Governments and health insurers use pooled funds to purchase health benefits for their citizens or insured populations. Health benefit packages are the collection of health prevention, treatment, care and rehabilitation services which are provided to these populations. They vary in scope from scheme to scheme and country to country. Definitions of what is included or excluded can be either very loose or very detailed.
Just because a citizen or an individual and their family have financial protection through insurance or a tax-funded financing scheme, does not mean that they have access to all of the services they might need.
The World Health Organisation have developed the Universal Health Coverage Cube. This shows that to extend the coverage you have to increase the proportion of the population covered, increase the range and scope of costs that are covered, and extend the service coverage.
Many countries moving toward Universal Health Coverage have started to develop lists of Essential Health Benefits or Essential Health Services. Sometimes these are known as Priority Health Benefits Packages.
What are the 8 Principles of Priority Setting?
According to the World Health Organisation, principles of Essential Health Benefits Package Design are summarised as:
- be impartial, aiming for universality
- be democratic and inclusive with public involvement, also from disadvantaged populations
- be based on national values and clearly defined criteria
- be data-driven and evidence-based, including revisions in light of new evidence
- respect the difference between data, dialogue, and decision
- be linked to robust financing mechanisms
- include effective service delivery mechanisms that can promote quality care
- be open and transparent in all steps of the process and decisions including trade-offs should be clearly communicated
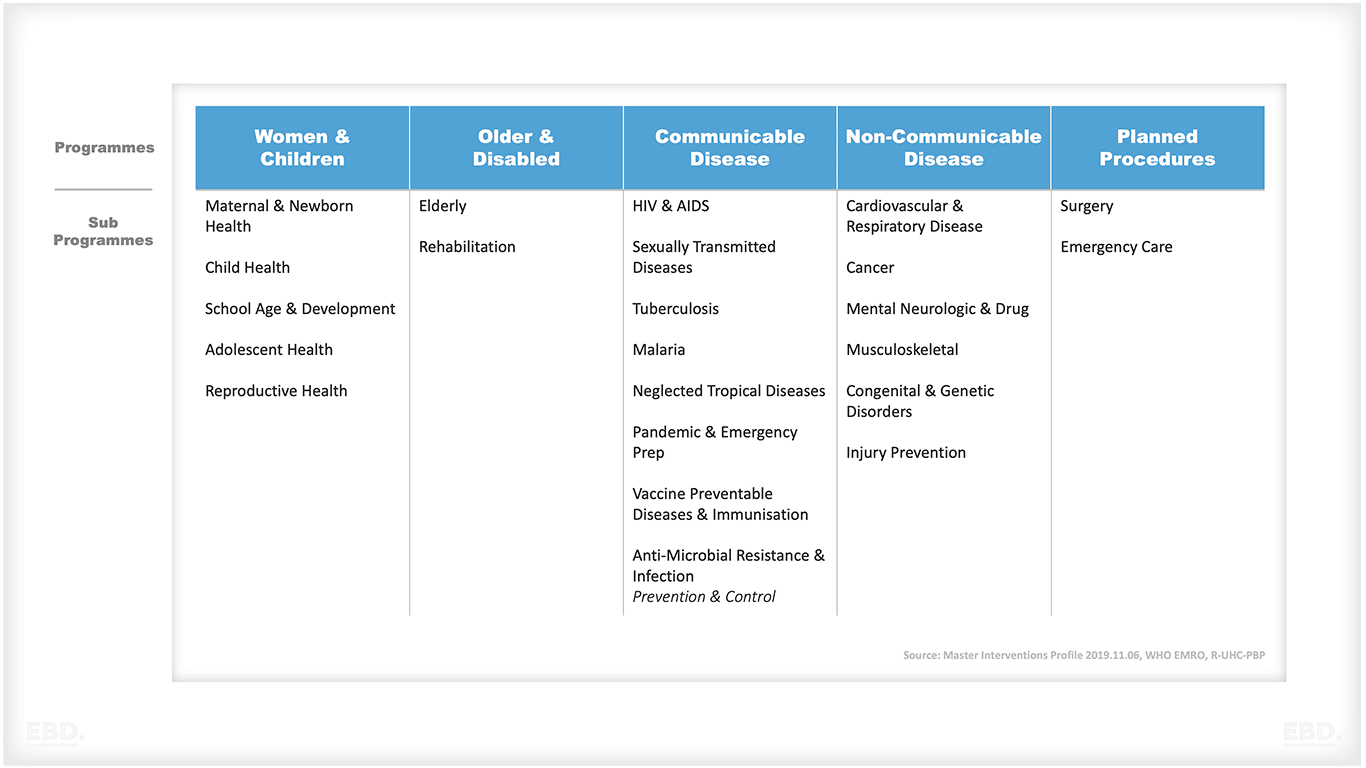
Health Benefits Package Frameworks
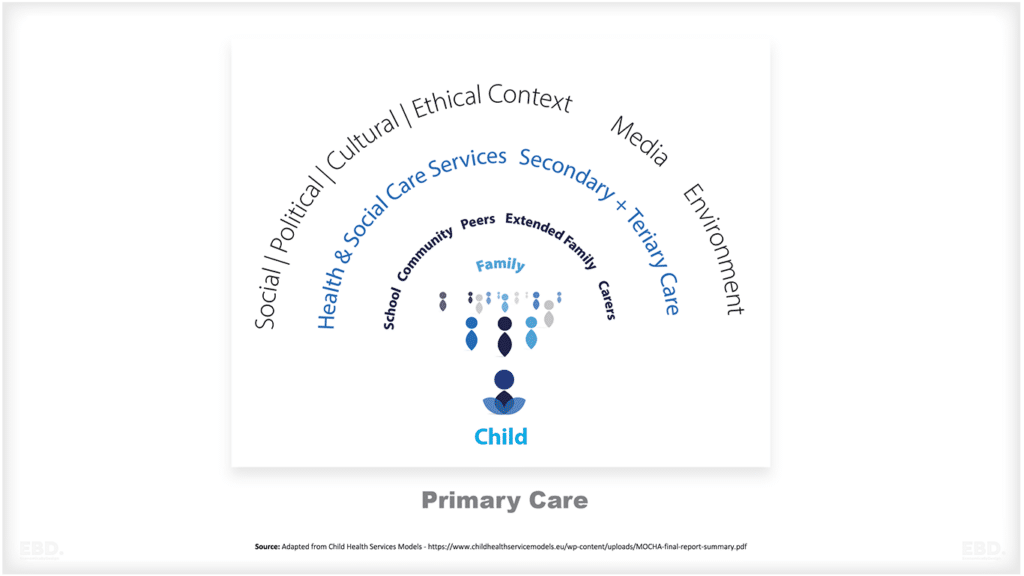
Often, health benefits packages are organised as programmes or classifications. These can be based on stages of the life course, risks and disease groupings, settings of care (primary, secondary, tertiary), or some combination.
Below is an example from the development of an Essential Health Benefits Package in Sudan.
The development of a list of priority benefits can be informed by evidence about population health needs based on the burden of disease, and a review of the cost, quality and availability of current services.
Proposals to change or expand current service provision should then be informed by evidence regarding intervention effectiveness and value for money of existing and new services, and an assessment of investment priorities within an envelope of funding.
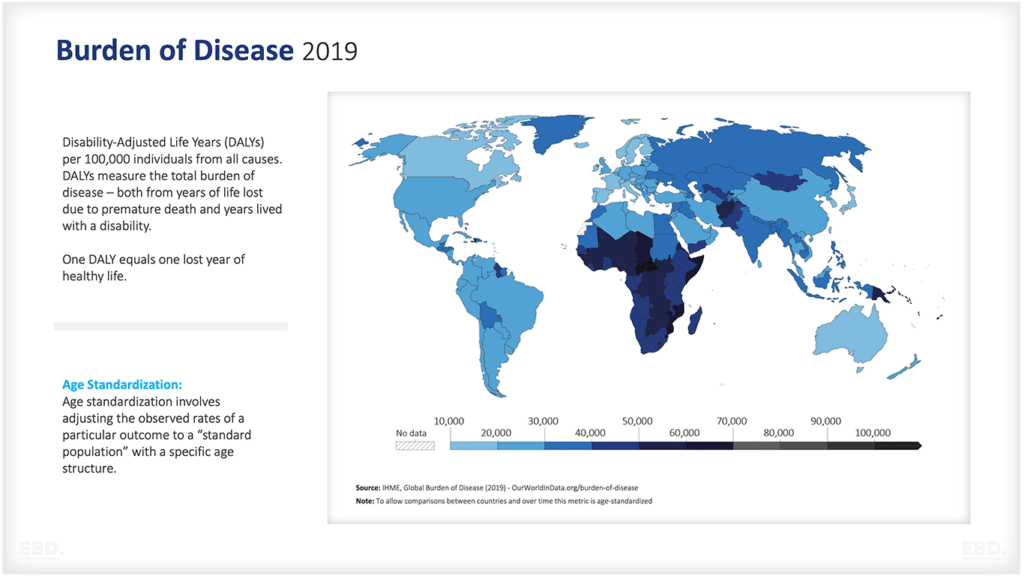
Burden of Disease
The burden of disease helps to identify health needs and priorities. The Global Burden of Disease (GBD) study is the most comprehensive attempt to date to quantify the global, regional, and national levels of diseases, injuries, and risk factors.
Disability Adjusted Life Years (DALYs) is a measure of the overall disease burden, combining premature death and ill-health. According to the GBD 2019 study, the 10 leading causes of DALYs globally are:
- Neonatal disorders
- Ischaemic heart disease
- Stroke
- Lower respiratory infections
- Diarrhoeal diseases
- Chronic obstructive pulmonary disease (COPD)
- Road injuries
- Diabetes
- Low back pain
- Congenital birth defects
The Institute for Health Metrics and Evaluation (IHME) provides an online visualisation tool that allows users to examine and compare the burden of disease by gender, age, year and location.
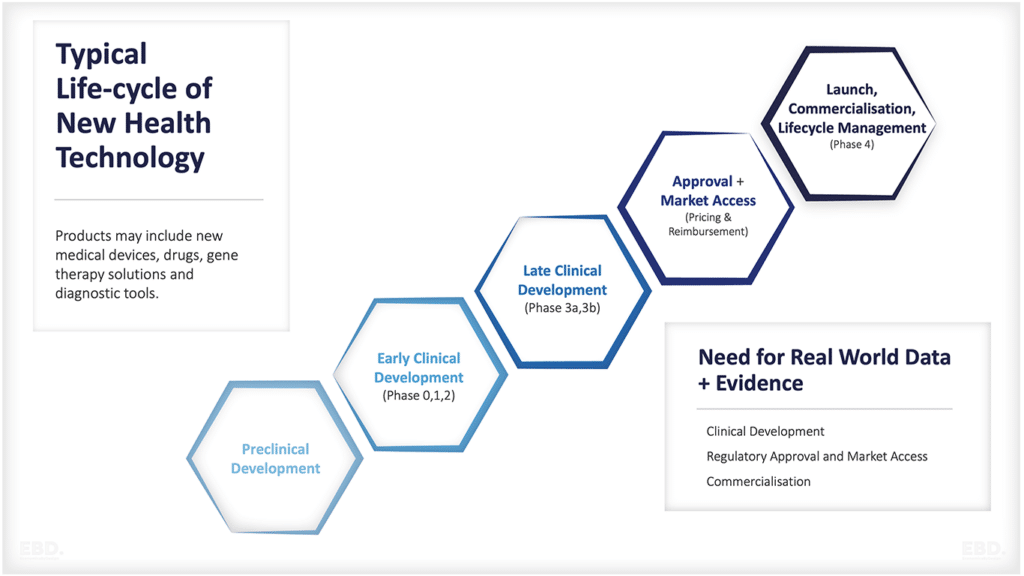
Effective Health Intervention Programmes and Services
Once the burden of disease has been established, the next step is to identify effective health intervention programmes and services that:
- are based on the best available evidence that there is a relationship between the health interventions and health outcomes
- take into account the preferences of patients and caregivers
- and are safe and feasible to deliver
There are many ways to identify and assess effective interventions. One way is to use systematic reviews, which are a type of literature review that uses predefined methods to identify, appraise, select and synthesize the findings of similar but separate studies.
Systematic reviews are considered to be the best source of evidence about the effectiveness of health interventions. However, they can be time-consuming and expensive to produce, and there may be a lack of high-quality evidence for some types of interventions, particularly in low-and middle-income countries.
An alternative approach is to use ‘rapid reviews’, which are a type of literature review that uses simplified methods to identify, appraise and synthesize the findings of similar but separate studies. Rapid reviews can be conducted in a shorter time frame and at a lower cost than systematic reviews, making them more feasible for resource-limited settings.
Cochrane Collaboration
The Cochrane Collaboration is a global network of over 37,000 people from more than 130 countries who work together to produce high-quality, up-to-date evidence about the effectiveness of health interventions. Cochrane reviews are considered to be amongst the highest quality evidence about the effectiveness of health interventions.
Joanna Briggs Institute
The Joanna Briggs Institute (JBI) is another global organisation that produces high-quality evidence about the effectiveness of healthcare interventions. JBI has developed a methodology for conducting rapid reviews, called the JBI Rapid Review Methodology (JBI RRM).
Disease Control Priorities Network
The Disease Control Priorities Network (DCP3) is a project that aims to provide decision-makers with the best available evidence about cost-effective interventions to improve health. DCP3 covers a wide range of conditions and interventions, and provides information on the costs, effects and cost-effectiveness of different interventions.
Outputs can be used across the world, particularly low to middle income countries, to help inform priority setting and development of Essential Packages of Health Services.
Value for Money
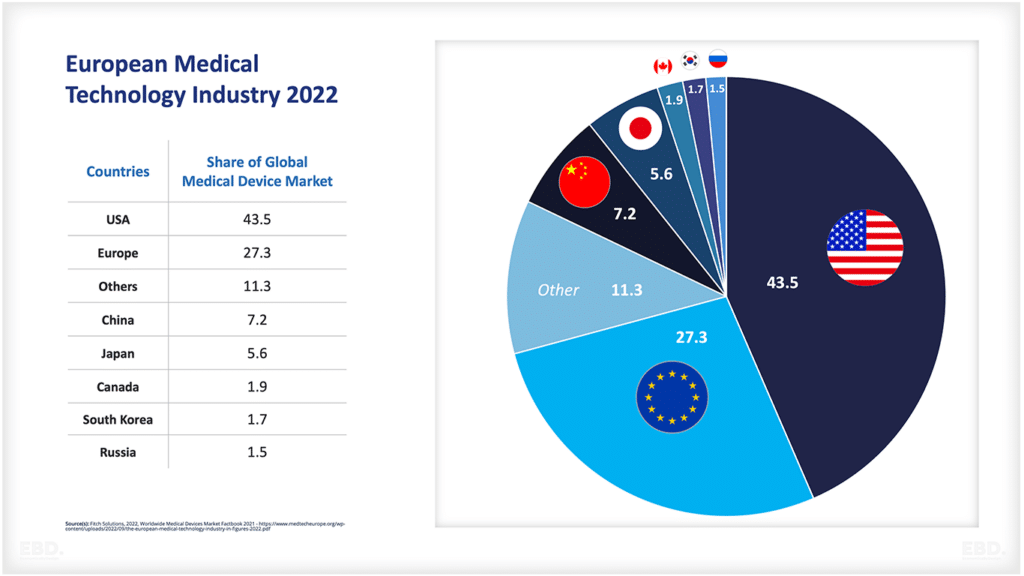
The costs and benefits of different treatment interventions are likely to vary country by country. Local pay rates, costs of infrastructure, supply chains, and economic circumstances which dictate the affordability of imported drugs and medical devices mean that the context for investment varies considerably.
There are, nonetheless, international databases which can be used as a starting point. An example is the TUFTS Cost-Effectiveness Analysis Registry which is a database that contains over 10,000 cost-effectiveness analyses from around the world. The registry includes studies on a wide range of topics, including HIV/AIDS, tuberculosis, maternal and child health, non-communicable diseases, and health system strengthening. which provide information on the costs of health interventions.
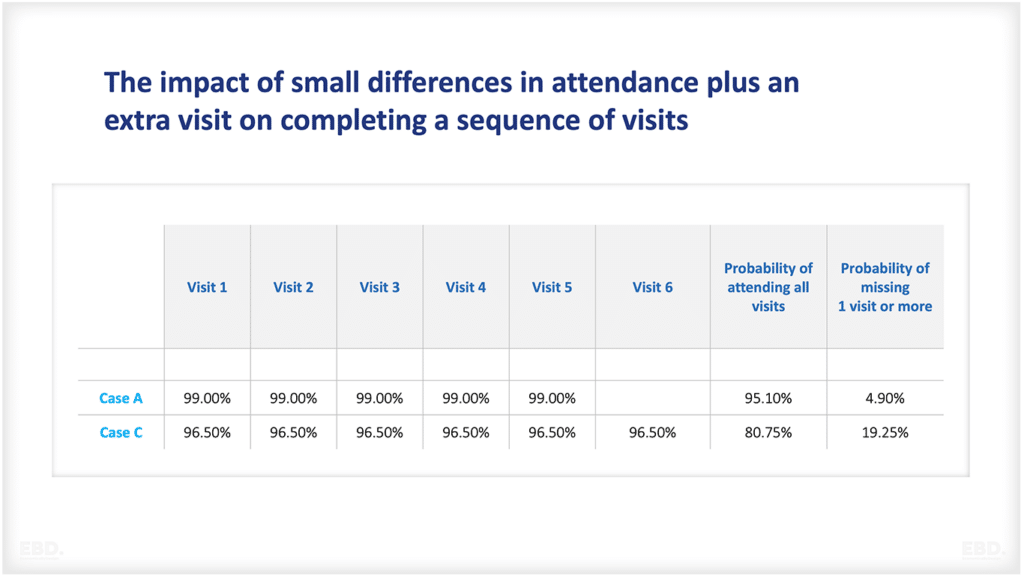
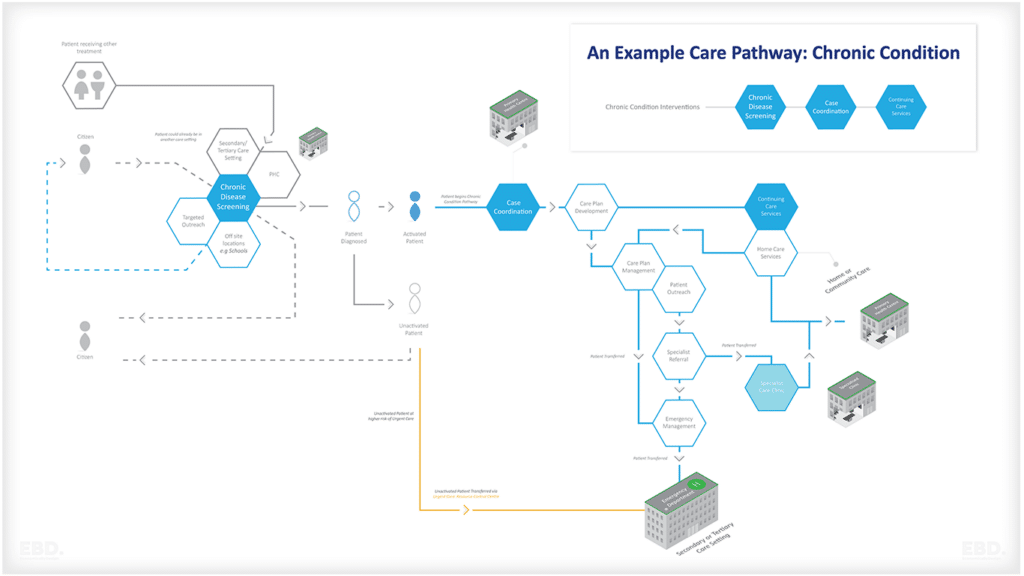
The Importance of Pathways or Programmes of Care
To improve health outcomes, health interventions must be delivered as part of a pathway or programme of care. This means that different interventions are delivered in a way that is coordinated and integrated, and that takes into account the needs of the individual patient.
Pathways or programmes of care can be delivered at different levels, from primary care (for example, community health worker programmes) to tertiary care (for example, cancer treatment programmes). Ideally, they need to cover prevention, diagnosis, treatment, management and rehabilitation.
Institutional Arrangements
Defining Essential Health Benefits is not a one-off exercise. Those responsible for purchasing health services use a system of ongoing monitoring, evaluation and review to keep the list relevant and up-to-date. This normally involves some form of governance arrangement which ensures that all stakeholders can participate in the decision-making process.
This will include, for example, public health and clinical experts, health service provider organisations, citizens and patients, and those responsible for system finance. The process needs to be transparent, and there should be mechanisms in place to ensure accountability for decisions.
An Example: The Affordable Care Act 10 Essential Health Benefits
The Affordable Care Act in the US, which was passed into law in March 2010, included a requirement that all health insurance marketplace plans in the individual and small group markets offer a comprehensive package of items and services – including 10 Essential Health Benefits:
- Ambulatory patient services
- Emergency services
- Hospitalization
- Maternity and newborn care
- Mental health and substance use disorder services, including behavioural health
- Prescription drugs
- Rehabilitative and habilitative services and devices
- Laboratory services
- Preventive and wellness services and chronic disease management
- Pediatric services, including oral and vision care
The Affordable Care Act 10 Essential Health Benefits were based on the list of benefits that were required to be covered by state law in at least some states as of March 23, 2010. The specification of the 10 essential benefits is at a very high level.
Before the Affordable Care Act, many people buying health insurance coverage did not have access to all of these benefits. For example, 1 in 3 people didn’t have coverage for substance misuse services. Around 10% of the population didn’t have coverage for prescription drugs. Close to 20% of people didn’t have coverage for mental health care.
Some plans do not have to follow the Affordable Care Act. For example, some states allow short-term policies and these often don’t include coverage for elements of these essential services. For example no diagnosis or treatment for AIDs or other immunodeficiency disorders.
What Prevents Countries from Providing Essential Health Services?
There are several barriers to providing Essential Health Services. These barriers can be divided into three main categories: financial, logistical, and political.
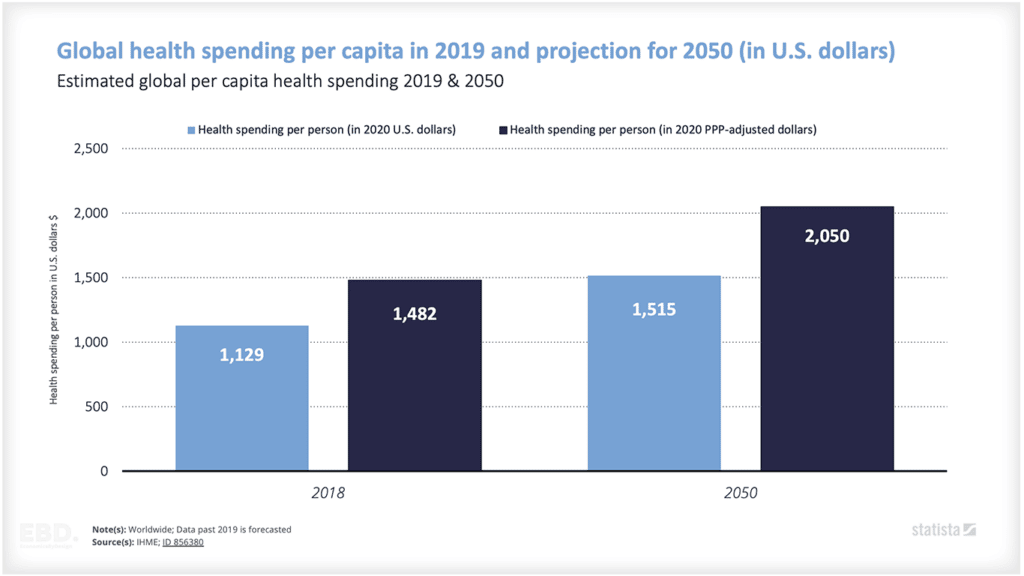
Financial barriers include the cost of providing essential health services. For example, the cost of vaccines can be a barrier to immunization. The cost of medicines can also be a barrier to treatment.
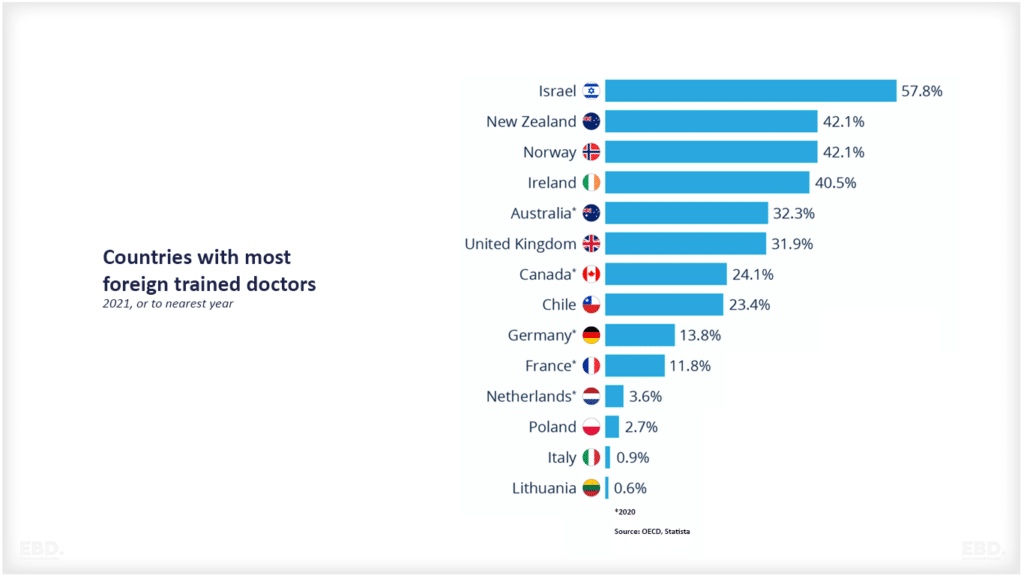
Logistical barriers include the lack of infrastructure and trained personnel. For example, many developing countries do not have the infrastructure to store or distribute vaccines. In addition, many developing countries do not have enough trained personnel to provide essential health services.
Political barriers include the lack of political will to provide essential health services. For example, some governments may be reluctant to provide essential health services because they are seen as a waste of money. Others may be reluctant to provide essential health services because they are seen as a way to control the population.
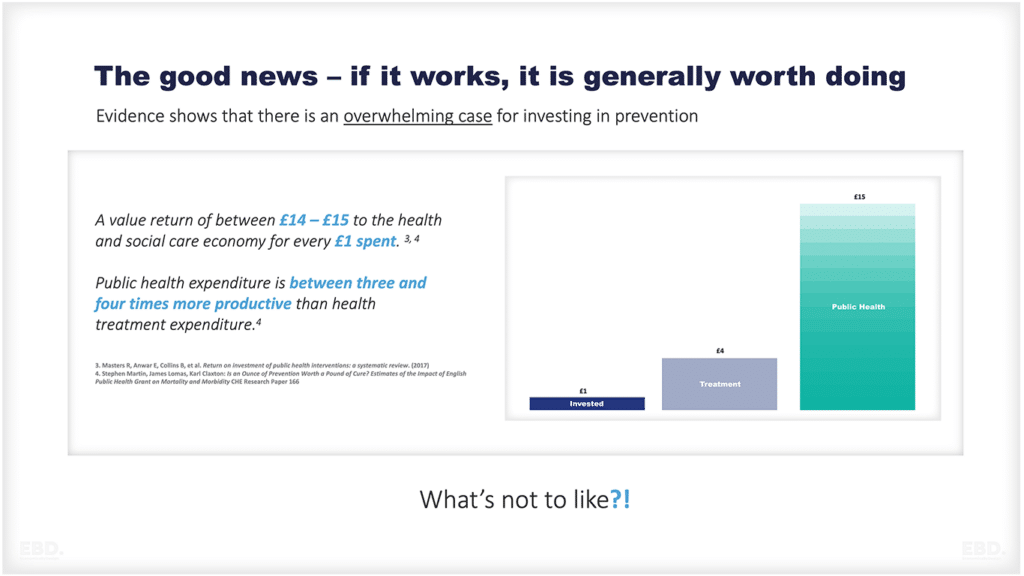
What is the Health Economic Value of Essential Health Benefits?
Essential Health Benefits are a critical investment in the health of a population. They not only save lives, but they also have the potential to reduce healthcare costs and improve economic productivity.