Integrated Care Systems: Introduction
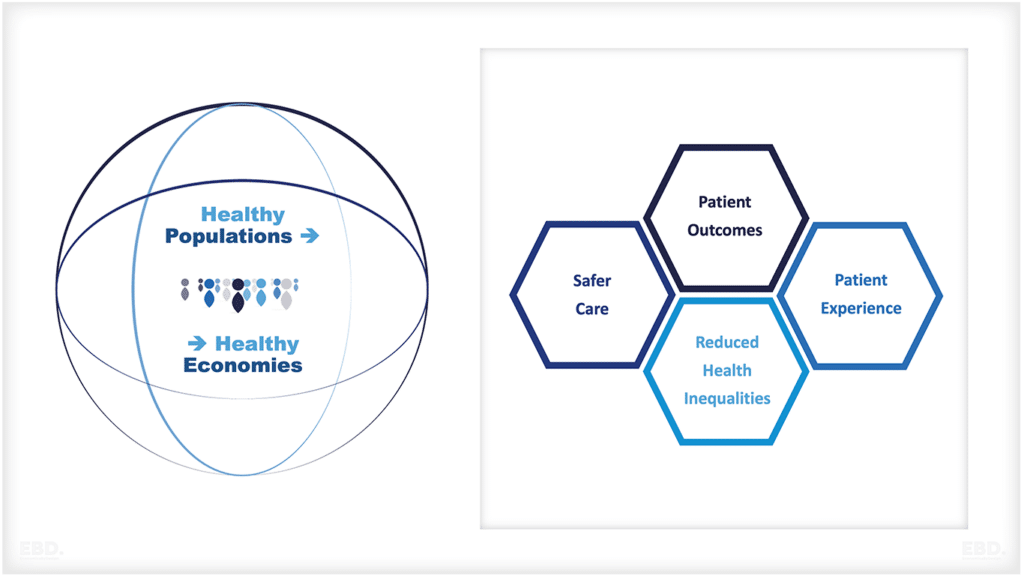
Across the world, there is a growing consensus that Integrated Care and People-Centred Care have the potential to deliver significant improvements in the value of health systems.
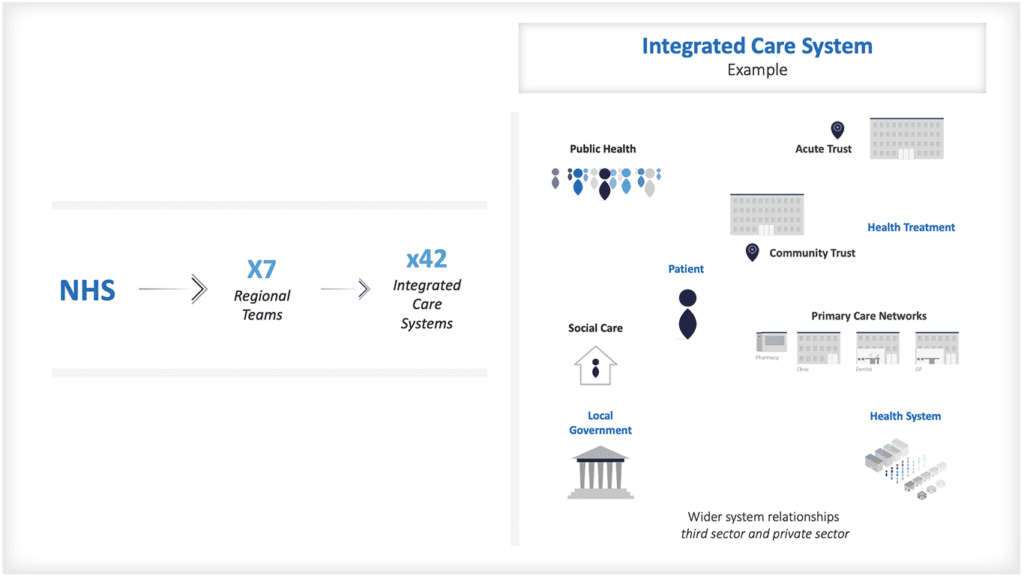
The NHS in England is currently investing heavily in the development of 42 Integrated Care Systems. (Integrated Care Systems & Financial Flows)
But what is the evidence to support this?
Integrated People Centred Health Services
Before we start let’s consider what integrated care systems are all about.
The Integrated People Centred Health Services Framework was adopted at the 69th World Health Assembly in 2016 and has been growing in influence across high, middle and low income countries alike.
Definition: Integrated Health Services
The Integrated People Centred Health Services framework definition is:
“Health services that are managed and delivered so that people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease-management, rehabilitation and palliative care services, coordinated across the different levels and sites of care within and beyond the health sector, and according to their needs throughout the life course.”
Strategies for Integrated Care Systems
There are five Integrated People Centred Health Services strategies:
Features of Integrated Care Systems Approaches
The implementation approach needs to be developed in the context of the country and local conditions; key features of successful implementation are that it should be:
- Country-led
- Equity focused
- Participatory
- System strengthening
- Evidence-based practice
- Results oriented
- Ethics based
- Sustainable
The Integrated People Centred Health Services Framework has some wonderful repositories of guidelines, good practice, and case studies and well worth taking a look.
International Foundation for Integrated Care (IFIC)
The International Foundation for Integrated Care also has a fabulous repository of evidence including the journal.
The IFIC 9 Pillars of Integrated Care
The IFIC 9 Pillars of Integrated Care (Lewis and Ehrenberg 2020) have been developed based on knowledge assimilated across a global network of over 20,000 IFIC members and have been complied to accelerate adoption of integrated care as health and care systems recover and rebuild following COVID-19.
They include:
- Shared Values and Vision emphasising the need for population health and service integration to be seen as a system-wide responsibility with all stakeholders committed to working together for a shared vision.
- Population Health and Local Context promoting the development of place-based initiatives designed around local needs, community assets and multi-sectoral approaches.
- People as Partners in Care building on from the concept of empowering patients, families and carers in the development of population health.
- Resilient Communities and New Alliances the importance of community assets and social and community capital as a driver for the effective community-based integrated care.
- Workforce Capacity and Capability highlighting the need for core-competencies and integrated working practices focused on patient advocacy, communication, inter-disciplinary working, people-centred care and continuous learning.
- System-Wide Governance and Leadership promoting network governance models which take into account the complexities and inter-dependencies of health systems and promoting co-operation rather than competition.
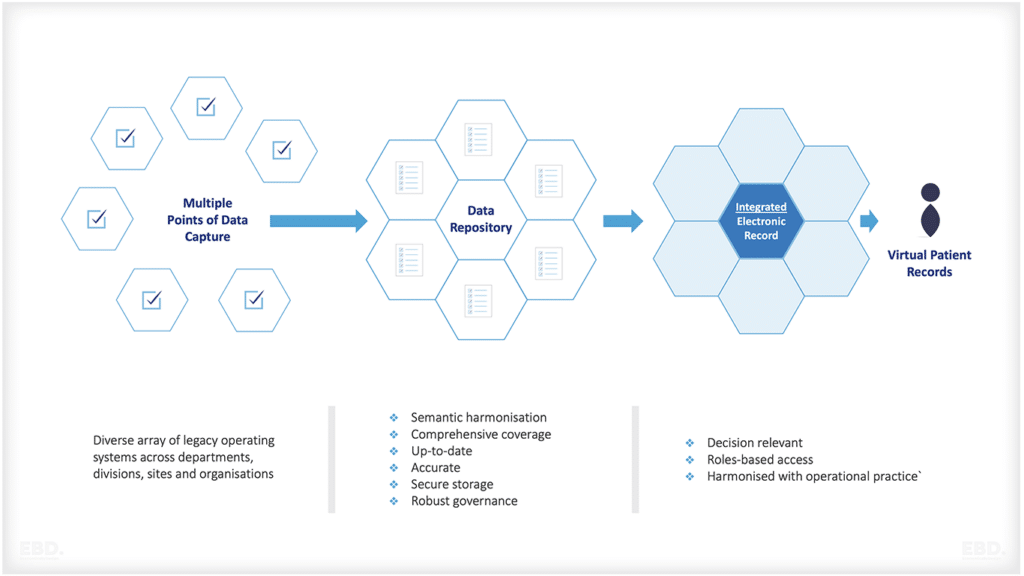
- Digital Solutions as the “cement” that holds the integration building blocks together, from infrastructure, through to shared care records and digital health technologies, to improve the monitoring, management and delivery of care.
- Aligned Payment Systems the use of payment systems as tools for enabling funds to flow where they need to and driving these as integration rather than as inhibitors, or providing perverse incentives.
- Transparency of Progress, Results and Impact there is no single model of integrated care that fits all systems; good practice should involve sharing results in a transparent and honest way to promote continuous learning.
The Knowledge Tree based on the 9 pillars has pre-curated links to articles and publications relevant to the evidence base for integrated care systems. If you are searching for evidence, it is worth starting here.
How good is the evidence base?
Sadly, though, despite lots of articles and papers, it is not easy to navigate or summarise the evidence. The evidence landscape is complex and depends as much on the quality of the research as it does on the quality of the model of integration being studied.
There are lots of case studies of good practice, and even where they have been well researched, they are all very different and results vary dependent on culture, geography and the characteristics of the local health and care systems.
Put bluntly, there isn’t a simple model of integration which can be copied for spread and adoption.
Let’s take a peek at three systematic reviews of the global evidence of the value of integrated care and what they each concluded.
New models of integrated care: evidence base
Our first review from a recent study funded by the National Institute of Health Research, looked at the evidence of new models of integrated care in developed countries: Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Understanding new models of integrated care in developed countries: a systematic review. Health Serv Deliv Res 2018;6(29).
The Baxter team undertook a systematic review of the published international literature to find out about the different types of integrated care interventions, how they worked, what outcomes they achieved and what impact they had.
Types of integrated care interventions
There is a huge variety of interventions which come under the umbrella of integrated care and the study by Baxter et al (2018) identified the following core types:
- joint assessment
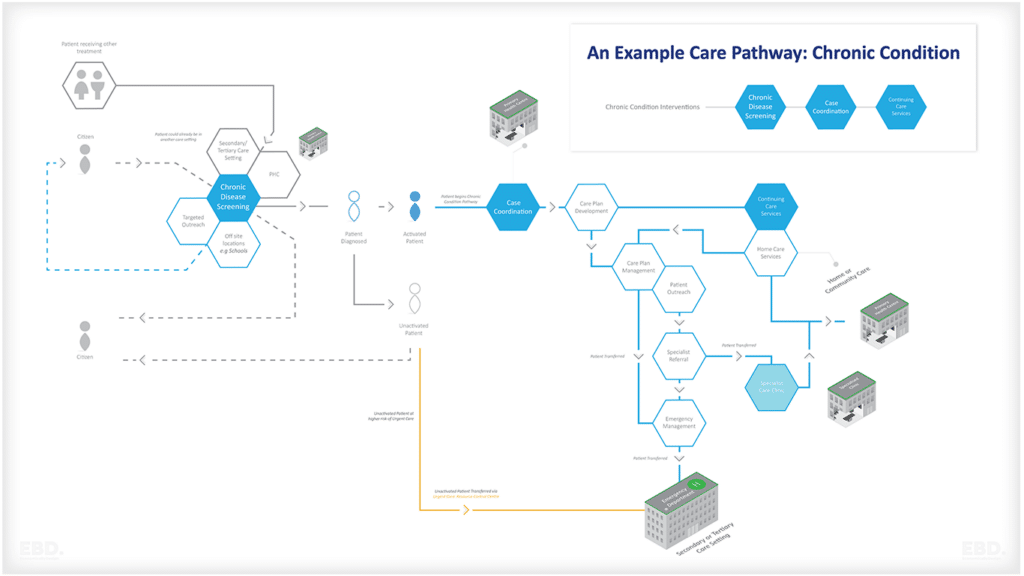
- integrated care pathways
- shared / agreed referral criteria
- care coordination
- joint reviews / discharge
- integrated information technology and patient records
- new services
- multidisciplinary teams
- relocating / repurposing staff roles
- joint commissioning
- financial integration
- organisational integration
Of these, the most frequently cited were integrated care pathways and the use of multidisciplinary teams.
Evidence of impact
As is often the case with complex interventions, the evidence of the impact of these interventions on patient outcomes, staff experiences and operational efficiency was difficult to interpret and generalise. But the review did conclude that new models of integrated care may:
- increase patient satisfaction,
- improve perceived quality of care
- improve access to services.
Integration at the Primary Secondary Interface
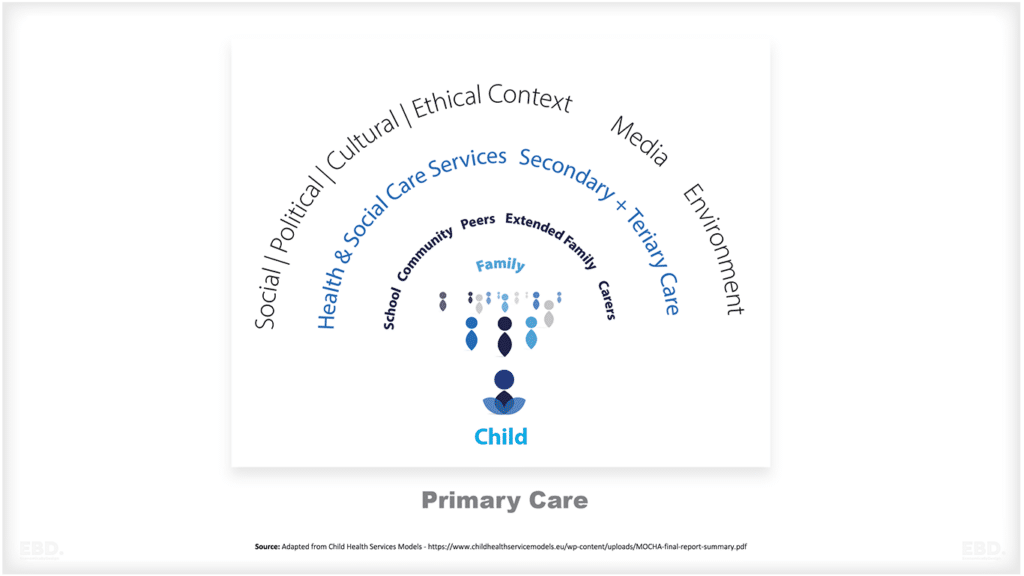
One of the biggest issues in healthcare is the interface between primary care and specialist clinical services. We all have experiences of having problems with the transition from primary care to secondary care (referral) and back again (management and discharge). One important aspect of integration must be to improve care coordination between these two sets of health care professionals and often the two settings of care.
But what does the evidence say?
In 2015, a study was published in the Australian Journal Of Primary Health: Geoffrey K. Mitchell, Letitia Burridge, Jianzhen Zhang, Maria Donald, Ian A. Scott, Jared Dart and Claire L. Jackson: “Systematic review of integrated models of health care delivered at the primary–secondary interface: how effective is it and what determines effectiveness?”.
The team did a systematic review of the international literature to specifically look at vertical integration for the management of chronic/complex diseases for individual patients.
What features facilitated improvements?
This team identified six elements that seemed to facilitate improvements in models of integrated care across the primary secondary divide:
- multidisciplinary teams
- communication and information exchange
- shared care guidelines and pathways
- training and education
- access and accessibility
- viable funding models
Evidence of outcomes
This review looked at economic outcomes. But these were only limited to costs and only covered a few studies. Results varied with some studies showing lower overall costs and others showing increased costs. Like many economic evaluations, the results depended on the starting point, the scope of the change, and the local geographical and health system context. The studies did however show modest increase in clinical outcomes and significant improvements in process outcomes.
Integrated care: costs and effects
Our last featured study was a systematic review of the costs and effects of integrated care, published in the European Journal of Health Economics (2020). Stephen Rocks, Daniela Berntson, Alejandro Gil‐Salmeron, Mudathira Kadu3, Nieves Ehrenberg, Viktoria Stein, Apostolos Tsiachristas “Cost and effects of integrated care: a systematic literature review and meta‐analysis” (2020).
This was a systematic review of the international literature focused solely on cost-effectiveness of integrated care.
Evidence of impact
This study showed lower costs and higher outcomes for integrated care systems across all regions covered (North America, Europe, Australia, Asia and Africa). What they found was that the impact on costs and outcomes were generally observed where studies were followed up over a reasonable period of time (at least more than a year). The benefits therefore take time to come to fruition.
What was really interesting was their findings that the results varied by type of integrated care intervention:
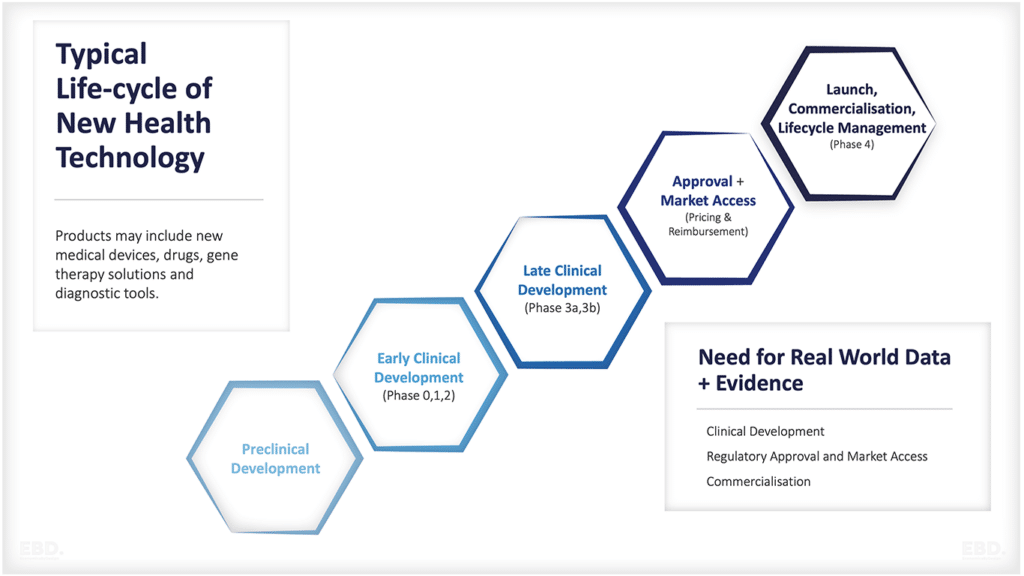
- disease management programmes reduced costs and increased outcomes
- integrated care teams reduced costs
- care coordination increased costs
- integrated care management improved outcomes
- integrated care pathways showed now change in costs or effects!
What Should We Make of The Evidence?
First and foremost is how difficult it is to do a systematic review of evidence for a concept.
Integrated care is an enormously broad topic with multiple definitions and applications. It’s rather like doing a systematic review of the impact of food on health – there is just too much variation and results will be meaningless.
What should we conclude from the evidence?
The paucity of comparable evidence doesn’t mean that integration as a concept is not worth doing, rather that there is no single model that we can generalise from.
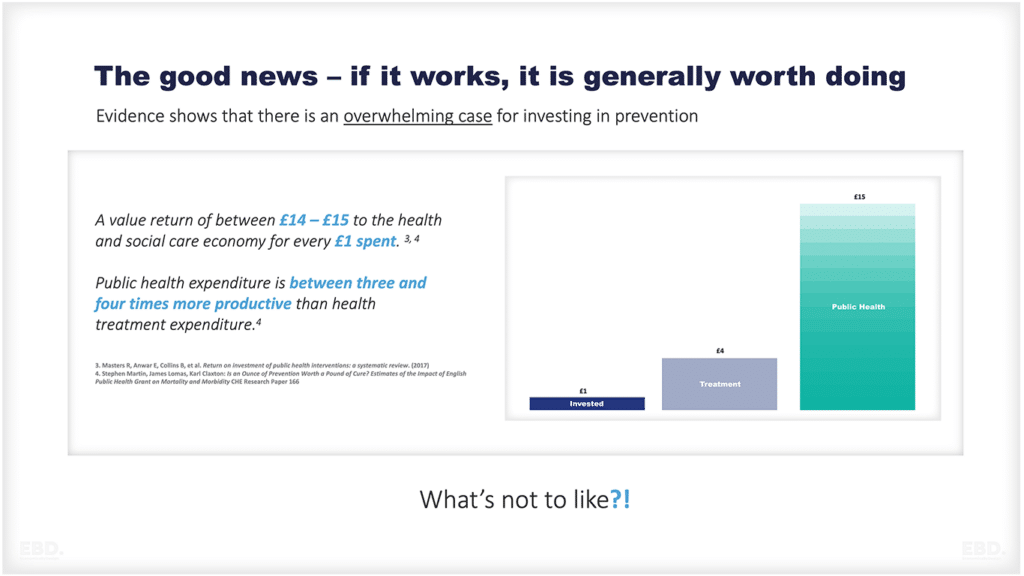
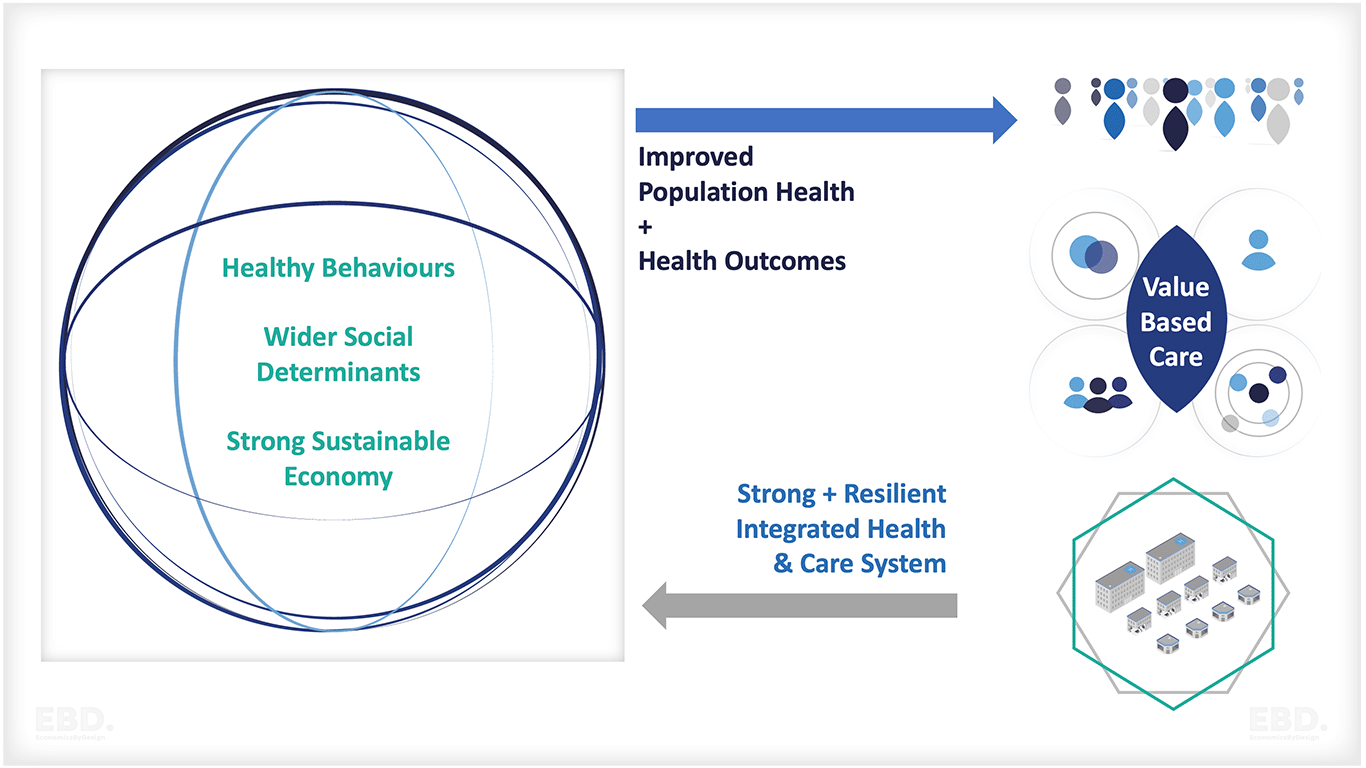
Moreover, despite all the problems, all three systematic reviews suggest that there is evidence that designing and implementing health care systems and services that are people-centred and integrated contribute to improved population health, patient outcomes and health system efficiency.
Integrated people-centred health services are also clearly a good thing from a theoretical perspective. And, it is an important component of wider population and economic health.
What is not to like?
What Should We Do About It?
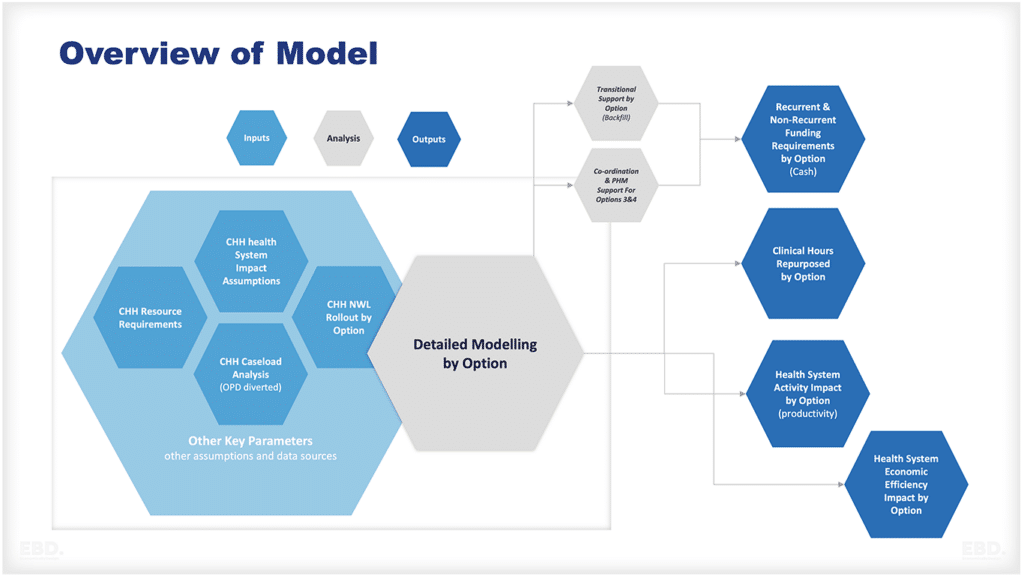
In practice, if you want to add value to the health and care system by improving integration you need to look at what is currently being done, how it can be improved, what it will cost, what the benefits will be, and whether we can afford it.
You can look to the literature for ideas. But is hard to simply copy a model that worked somewhere else in the world. Just because it was impactful somewhere else, does not mean it is right for your local circumstances.
This is really about designing value in from the beginning and then measuring achievement through evaluation afterwards – after all, informing the evidence base is probably helpful too!