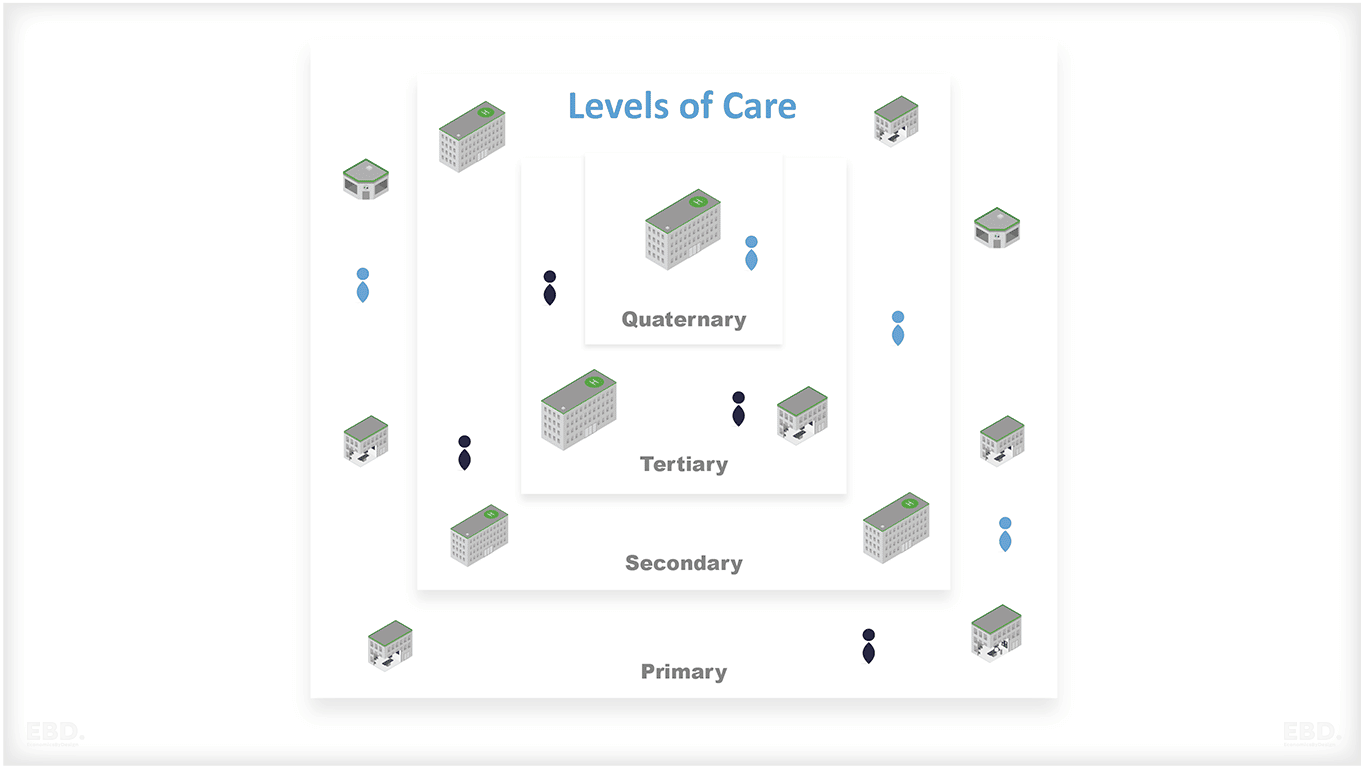
What are Levels of Care
Essential Health Benefits can be delivered at different levels within the health system.
Levels of care describe the severity of an issue and the kinds of health conditions the doctors treat as well as the specialities that they practice.
In this article, we look at the different levels of the healthcare system and how they relate to each other.
The 4 Main Levels of Care of a Healthcare System
In almost every health system the regional or national health system has different types of providers, each with its own set of services and specialities.
The different types of providers usually correspond to different levels of care within the health system. In general, these can be classified into four main categories:
1. Primary Care
2. Secondary Care
3. Tertiary Care
4. Quaternary Care
This article describes levels of care which involve different types of providers and what situations can require different levels of care.
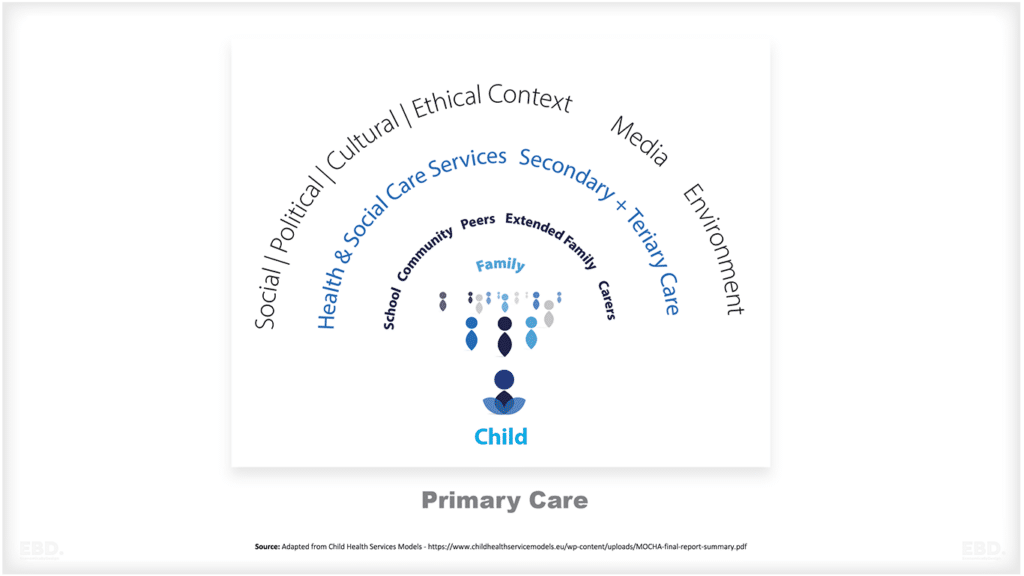
What is Primary Care?
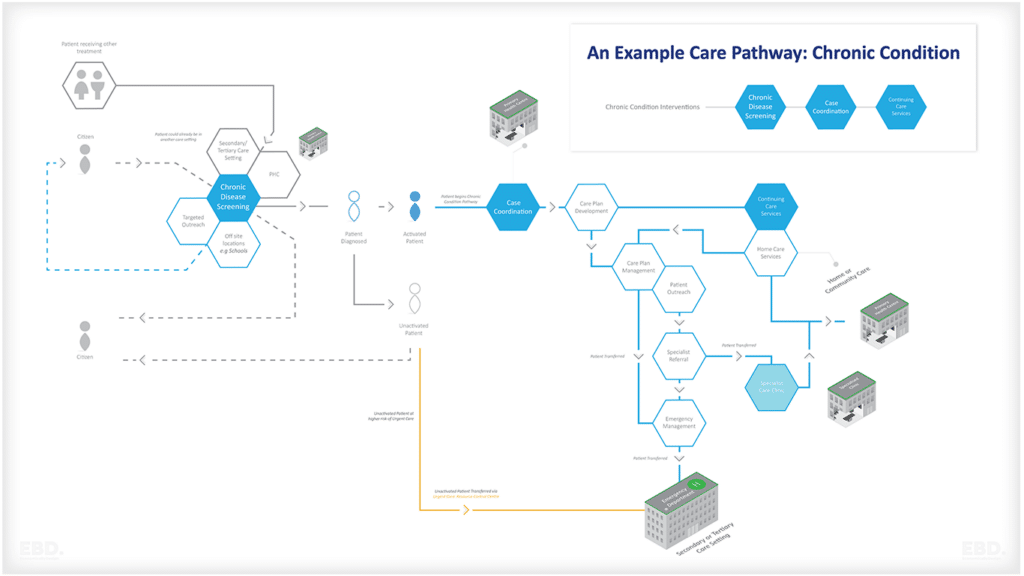
Primary care is the first contact that a patient has with the health system when they have a health problem.
What is the Difference Between Primary Care and Primary Health Care?
Primary Care is not to be confused with Primary Health Care (PHC), which is a more holistic approach to health that looks at all the factors that affect a person’s health. This includes access to safe water and sanitation, food security, education, and housing.
According to the World Health Organisation Primary Health Care has three components:
- Integrated health services to meet people’s health needs throughout their lives
- Addressing the broader determinants of health through multisectoral policy and action
- Empowering individuals, families and communities to take charge of their own health.
Primary care is an important component of PHC.
Who Provides Primary Care?
In most cases, primary care is provided by General Practitioners (GPs), although in some cases it may be provided by other health professionals such as nurse practitioners, physician associates or pharmacists.
General practitioners (GPs) are trained to deal with a wide range of common health problems. They are also trained to recognise when a patient needs to be referred to a specialist or another level of care. In many health systems, GPs provide the “front door” to other parts of the health system.
General practitioners are often known as family practitioners. This is in part due to their role in providing care for the whole family, from babies and children to adults and the elderly.
What Services are Provided in Primary Care?
Primary care services include :
- Health promotion and disease prevention
- Health education
- Diagnosis and treatment of acute and chronic diseases
- Management of chronic diseases
- Rehabilitation
- Palliative care
- Coordination of care for patients with complex health needs
How is Primary Care Organised?
There are several different models for organising primary care, which vary according to factors such as the health system, the geographical area, and the type of primary care practitioners involved.
The main models for organising primary care are:
Solo Practice
One GP working alone
Partnership
Two or more GPs sharing premises and staff
Group Practice
A number of GPs working together in one surgery
Health Centre
A group of practices sharing premises and staff, often with other health professionals such as nurses, community workers, and pharmacists
Network
A group of practices working together across a geographical area, often with other health and social care services
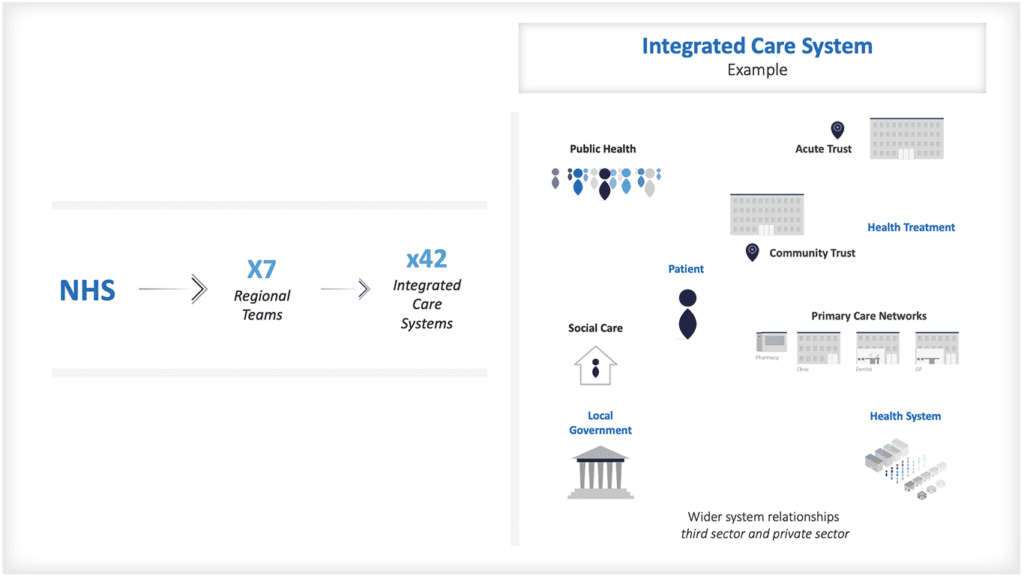
In England, in recent years Primary Care Networks (PCN) have become part of Integrated Care Systems. A Primary Care Network is a group of general practices working together with other local health and care services, to improve the health and wellbeing of the local population.
PCNs were introduced in England as part of the NHS Long Term Plan, and are a key part of how integrated care systems (ICSs) are being developed.
In many health systems patients enrol with a primary care practice, and are then able to receive care from that practice. In some cases, patients may be able to choose which primary care provider they enrol with, while in others they may be assigned to a provider based on their location.
Enrolment is often referred to as Empanelment. Patients may also be able to self-refer to some primary care services, without having to see their GP first, for example for sexual health.
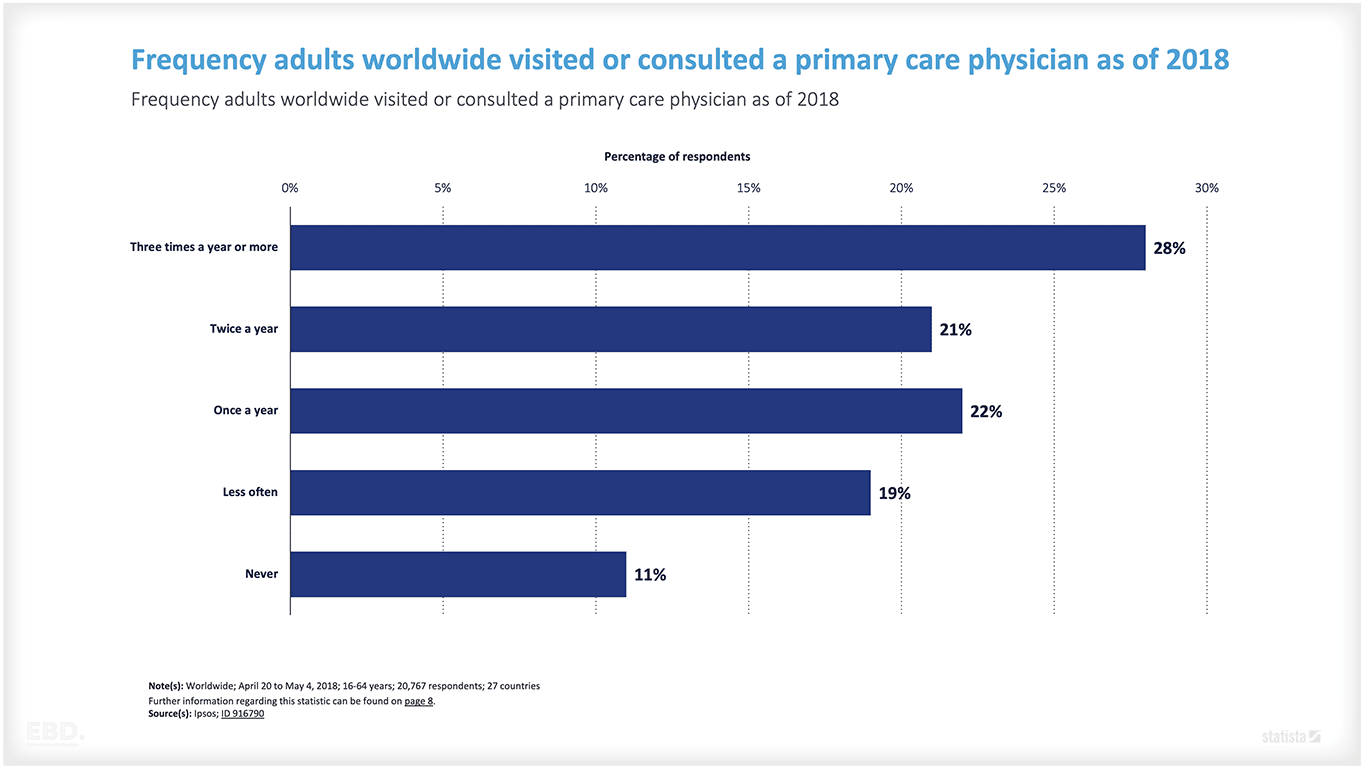
According to a global survey by Ipsos in 2018, 28% of adults (aged 16-64) visit a primary care physician three times a year or more. Only 11% of adults had never consulted a primary care physician.
How is Primary Care Paid For?
In most health systems, primary care services are financed through a mix of general taxation and specifically earmarked taxes or insurance premiums. In some cases, patients may also make a direct payment (co-payment) for some primary care services. Payment models often include a fixed amount per person covered plus variable amounts for particular services such as screening or health checks.
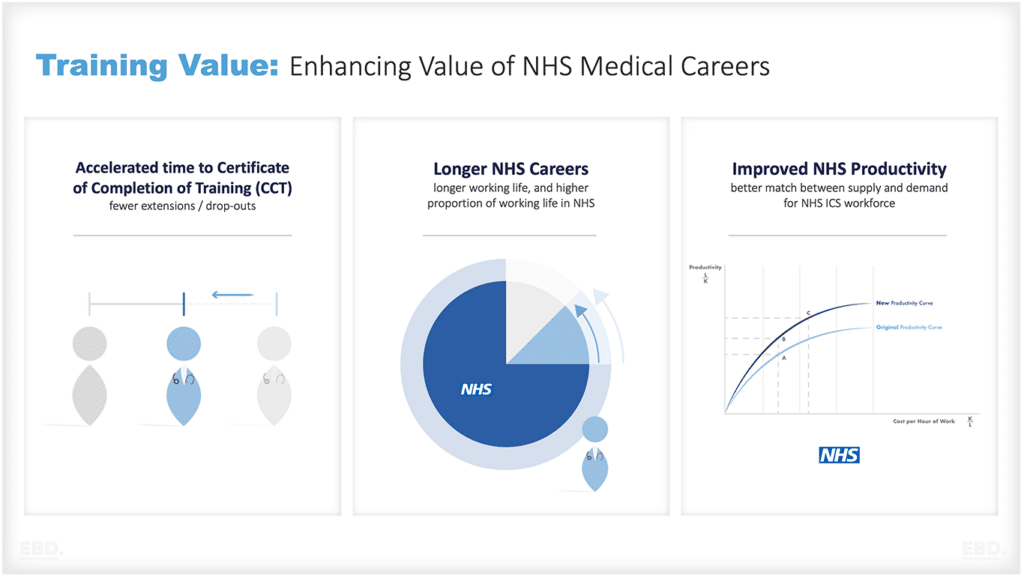
What is the Economic Value of Primary Care in the Health System?
Primary care plays a vital role in the health system, providing the first point of contact for patients and often acting as a gateway to other parts of the system.
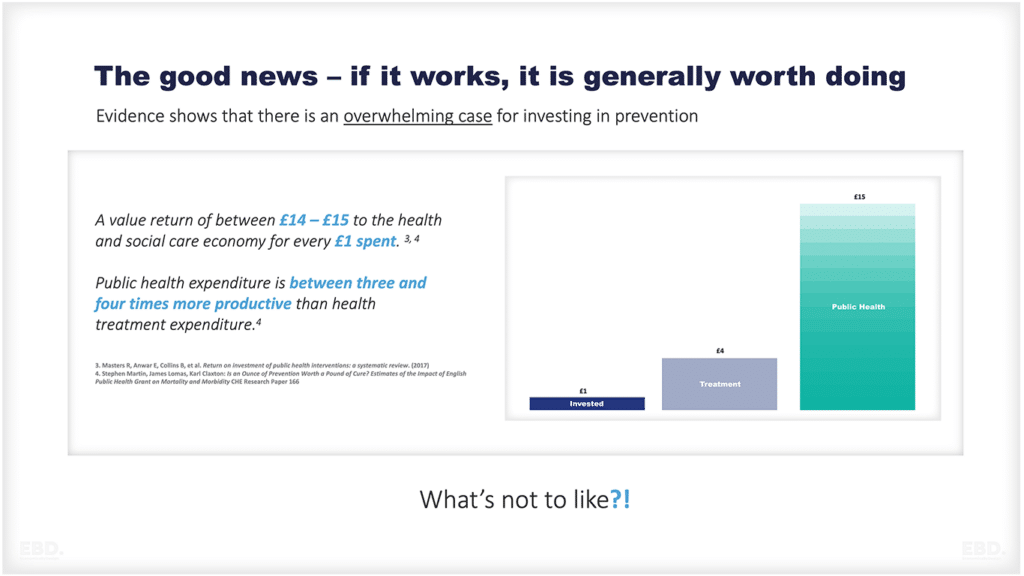
Primary care is often seen as a cost-effective way to deliver healthcare, due to its focus on disease prevention and management of chronic diseases. Primary care adds value by:
- Helping to prevent illness and promote health and wellbeing
- Providing early diagnosis and treatment of diseases
- Improving patient experience and satisfaction
- Reducing unnecessary hospital admissions
- Improving population health outcomes
This results in:
- Indirect cost savings from preventing or managing chronic diseases-
- Indirect cost savings from avoiding hospitalisations
- Economic value from longer healthy life expectancy and improved health and wellbeing
There is a large body of evidence that demonstrates the value of primary care in improving population health outcomes and reducing healthcare costs.
What are the Challenges Facing Primary Care?
Despite its importance, primary care is facing challenges in many countries. These challenges include:
- An ageing population and the consequent increase in chronic diseases and demand for services
- Severe workforce shortages and an under-investment in general practice training
- Ensuring effective vertical integration for the management of patient care with secondary and tertiary care
- Ensuring effective horizontal integration with other parts of PHC and social care
- The challenges of providing care for complex patients living with multiple chronic conditions.
These challenges mean that it is more important than ever to ensure that primary care services are high quality, efficient and sustainable.
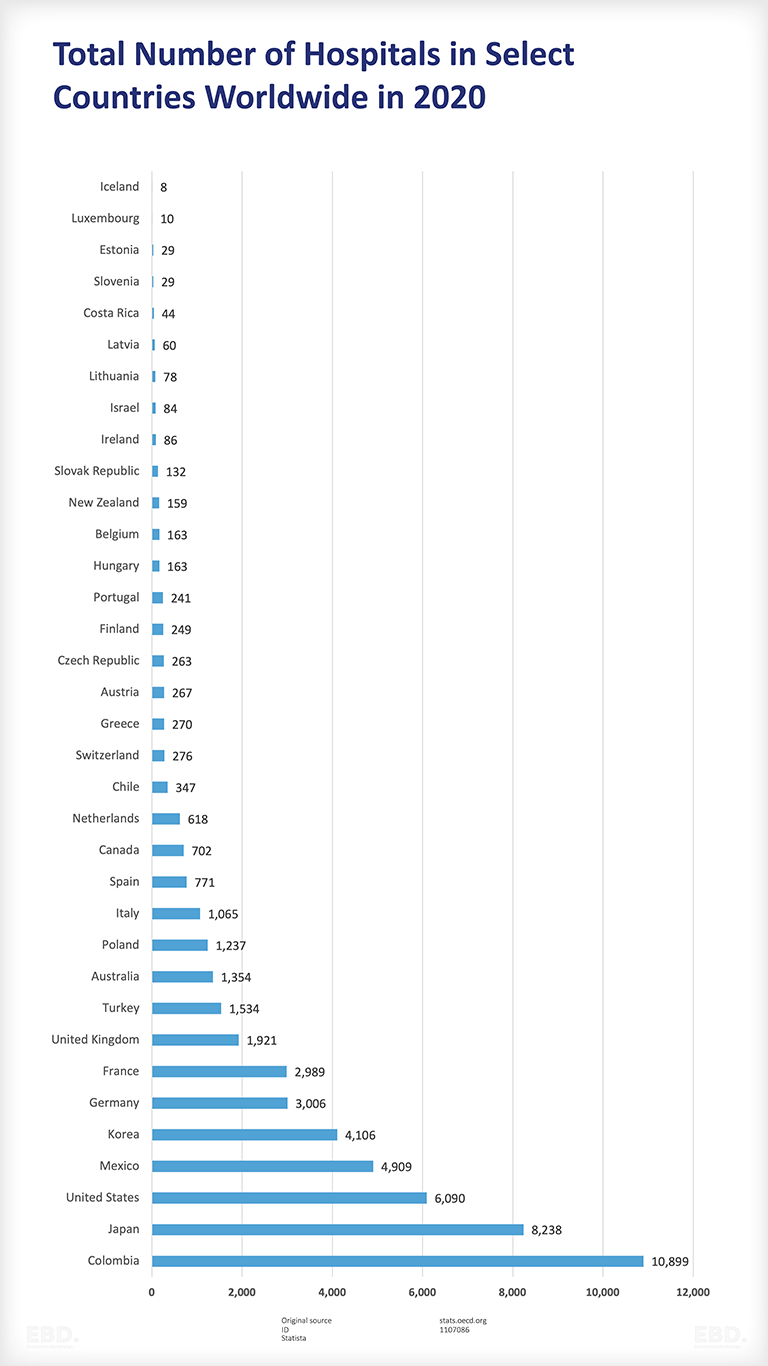
| Colombia | 10,899 |
| Japan | 8,238 |
| United States | 6,090 |
| Mexico | 4,909 |
| Korea | 4,106 |
| Germany | 3,006 |
| France | 2,989 |
| United Kingdom | 1,921 |
| Turkey | 1,534 |
| Australia | 1,354 |
| Poland | 1,237 |
| Italy | 1,065 |
| Spain | 771 |
| Canada | 702 |
| Netherlands | 618 |
| Chile | 347 |
| Switzerland | 276 |
| Greece | 270 |
| Austria | 267 |
| Czech Republic | 263 |
| Finland | 249 |
| Portugal | 241 |
| Hungary | 163 |
| Belgium | 163 |
| New Zealand | 159 |
| Slovak Republic | 132 |
| Ireland | 86 |
| Israel | 84 |
| Lithuania | 78 |
| Latvia | 60 |
| Costa Rica | 44 |
| Slovenia | 29 |
| Estonia | 29 |
| Luxembourg | 10 |
| Iceland | 8 |
What is Secondary Care?
Secondary care is the next level of care after primary care. Secondary care is defined as “the provision of medical care by specialists who generally do not have first contact with patients.”
This level of care is typically required when a patient has a condition that requires specialized treatment and/or monitoring.
Who Provides Secondary Care?
It is usually provided by specialists in hospitals or other settings such as community health centres. These specialists include surgeons, physicians, psychiatrists, and paediatricians.
The specialists are supported by multi-professional teams including nurse professionals, professions allied to medicine such as therapists, imaging professionals and scientists.
What Services are Provided in Secondary Care?
Secondary care services include:
Inpatient Care
When a patient is admitted to hospital for further investigation and treatment
Outpatient Care
When a patient attends a hospital or clinic for specialist diagnosis or treatment without being admitted to hospital
Day Case Surgery
When a patient has an operation that does not require an overnight stay in hospital
Patients present as emergencies to an emergency department, or as planned referrals or admissions. Emergency secondary care is required when a patient has an acute illness or injury that requires immediate treatment.
Ambulance services play an important role in the delivery of secondary care, transporting patients to hospitals for further treatment. Emergency ambulance services are typically provided by the national health service or a private provider.
Paramedics and other emergency medical technicians provide care to patients at the scene of an incident and/or during transport to hospital.
Secondary care is generally organised around specialities. Examples include:
- Emergency medicine
- General surgery
- General medicine
- Cardiology
- Ear nose and throat
- Gastroenterology
- Geriatrics
- Gynaecology
- Neurology
- Oncology
- Orthopaedics
- Obstetrics
- Opthalmology
- Paediatrics
- Respiratory medicine
- Urology
How are Secondary Care Services Organised?
The way in which secondary care services are organised varies between countries. In most countries, secondary care services are provided by several different providers including government health services, not-for-profit private hospitals, commercial private hospitals and private clinics.
Patients are typically referred to secondary care by their primary care physician. In some cases, patients may self-refer or be referred by another health professional such as a physiotherapist.
There are several different types of referral systems:
Open Access
Where patients can refer themselves directly to a specialist without first seeing their primary care physician
Gatekeeping
Where patients must see their primary care physician before being referred to a specialist
Selective Gatekeeping
Where patients can self-refer to some specialists but must see their primary care physician before being referred to other specialists.
Secondary care providers cover a larger catchment population than primary care. Often the size of the catchment population is determined by the requirements for access to specialist staff and the need for them to see a sufficient volume of patients to maintain their skills, expertise and experience.
Some hospital providers employ their specialist clinical staff. Others contract with professionals or professional agencies who provide their services on a fee-for-service basis.
How are Secondary Care Services Paid For?
Secondary healthcare is generally more expensive than primary care, due to the specialized nature of the services provided.
Secondary care services are typically paid for by government health insurance systems, private health insurance companies or out-of-pocket payments by patients.
In some countries, secondary care services are provided free of charge to all citizens. In other countries, patients may have to pay a co-payment or deductible for secondary care services.
Those responsible for the strategic purchasing of health services use all types of payment models are used to pay for secondary care services.
For government-run hospitals services are generally funded through devolved budgets based on departmental line item costs or a block grant.
For other hospitals, fee-for-service is a common form of payment model. Some integrated care models or accountable care models use capitation funding linked with performance or outcome payments.
What is the Economic Value of Secondary Care in the Health System?
Secondary care plays a vital role in the health system, providing specialist treatment and monitoring for patients with complex conditions. It has the potential for value improvement by:
- Improving patient outcomes by delivering effective care in a timely manner
- Improving the patient experience by delivering patient-centred care in a timely manner
- Reducing unit costs by delivering care efficiently across different health professionals and departments for diagnosis, treatment, and care
- Working collaboratively with primary care to ensure patients are managed in the community wherever appropriate
- Working effectively with social care providers to ensure patients who need on-going care but who are ready for discharge can return home, or to supported accommodation, as soon as possible.
There is evidence that integrated care models which seek to improve the coordination of care across different settings can lead to significant cost savings and improved patient outcomes.
What are the Challenges with Secondary Care?
There are several challenges associated with secondary care. Examples include:
- Waiting times – patients may have to wait a long time to see a specialist or to receive treatment
- Fragmentation of care – due to the number of different types of providers, it can be difficult for patients to receive coordinated care
- Lack of access – some patients may live in remote areas or have difficulty accessing transportation, which can make it difficult to get to appointments or to receive treatment
- Cost – secondary care services can be expensive, which may make them unaffordable for some patients who do not have access to insurance or tax-funded services
- Workforce issues – there may be a shortage of certain specialists, which can make it difficult for patients to receive the care they need.
What is Tertiary Care?
This level of care is typically required when a patient has a condition that requires very specialised treatment and/or monitoring.
Tertiary care facilities are usually found in large teaching hospitals or stand-alone centres that are affiliated with a hospital.
Common examples of tertiary care services include:
- Advanced complex diagnostics
- Specialist cancer management
- Transplantation surgery
- Cardiac surgery
- Neurosurgery
- Plastic surgery
- Advanced neonatology services
Referral of a patient to tertiary care is usually done by a secondary care specialist, although in some cases a primary care physician may refer a patient directly to a tertiary care facility.
Tertiary healthcare is generally even more expensive than primary or secondary care, due to the increasing complexity of the services provided.
Due to its specialist nature, tertiary healthcare covers a larger catchment population than secondary care and is often organised regionally with referrals managed through established links between tertiary and secondary centres.
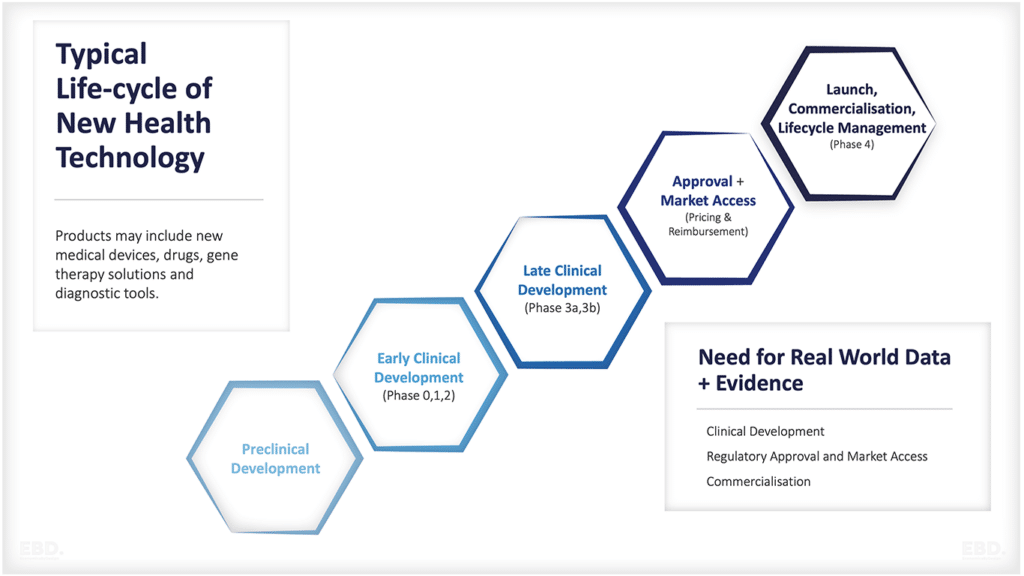
What is Quaternary Care?
Quaternary services are an extension of tertiary care. However, it’s very specialised and very uncommon and typically offered in only very limited national centres and international centres.
Quaternary care facilities are usually found in large teaching hospitals or stand-alone centres that are affiliated with a hospital. Services include:
- Treatment for rare or complex conditions
- Clinical trials for new treatments and medications
- Cutting-edge medical technology
- Rehabilitation after a serious injury or illness.
As with tertiary care, referrals are managed through established links between tertiary and secondary centres.
Education, Training and Research
All levels of care provide some level of education and training to healthcare professionals and provide important venues for health research and innovation.